Microsurgery & Replantation
Specialization
- Brachial Plexus
- Breast Surgery & Reconstruction
- Burns
- Burns
- Cancer Reconstruction
- Cleft Lip and palate
- Congenital Hand Differences
- Cosmetic Surgery
- Diabetic Foot & Chronic Wounds
- Hand and Wrist Surgery
- Lower Limb Reconstruction
- Lymphedema
- Maxillofacial Surgery
- Microsurgery & Replantation
- Microsurgery Lab
- Skin Bank
- Spastic Hand
- Super Speciality Courses & Fellowships
Microsurgery & Replantation
Microsurgery is the marvel of modern surgery. To put it simply, operating with a microscope is called microsurgery. Surgeons of various specialities like Plastic Surgery, ENT, Ophthalmology, Neurosurgery and many more use the microscope. All of them use the microscope to do whatever they were doing a lot better. After all, you do better when you see better.
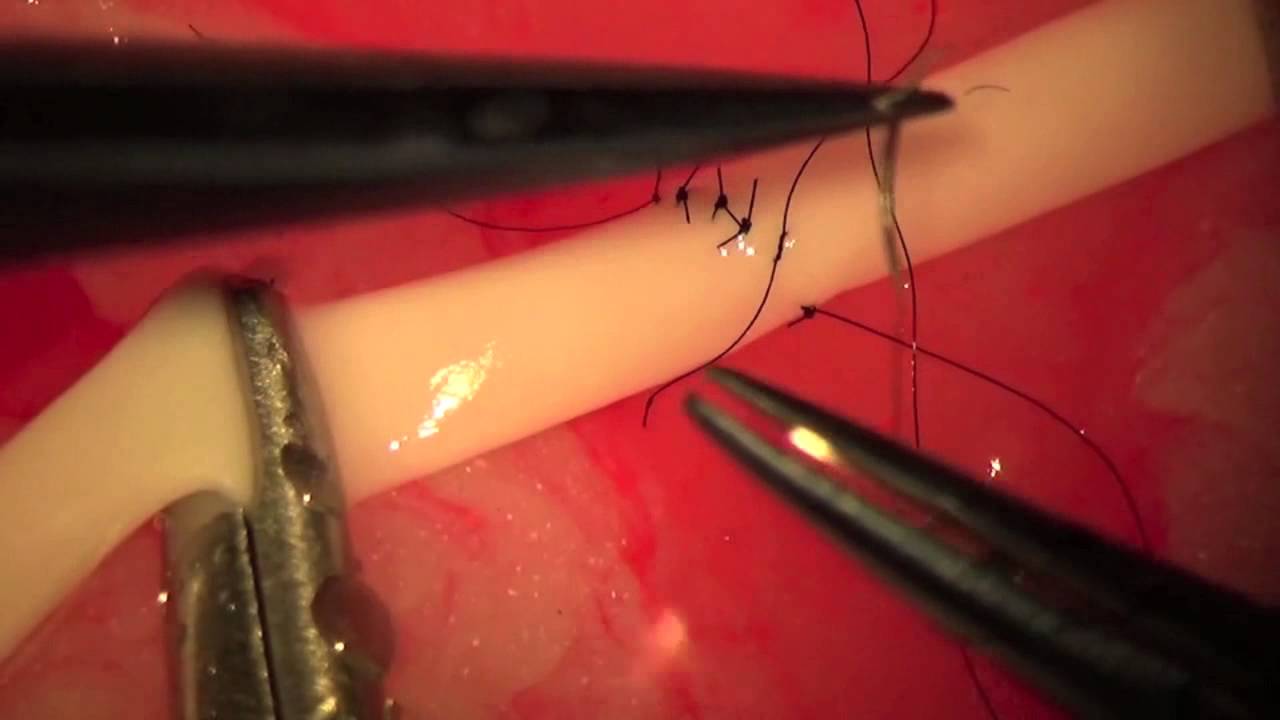
Plastic and Reconstructive surgeons took it a step further by fine-tuning the skills of joining small blood vessels, as small as or even lesser than a millimetre in diameter. That helped to revolutionise reconstructive surgery. Amputated fingers and hands were joined back. When major accidents resulted in large tissue defects, they were usually amputated. With the advent of microsurgery Plastic and Reconstructive surgeons were able to transfer tissues from one part of the body to another. This led to the salvage of severely injured hands and legs.
It is just not in trauma where microsurgery is used. The same capability is also used in the reconstruction of defects after removal of cancer, treatment of lymphedema, reconstruction of major defects left by burns and even in infectious conditions like the diabetic foot. The benefits are endless. The imagination, hard work, skills and dexterity of microsurgeons has opened up endless possibilities for the benefit of patients.
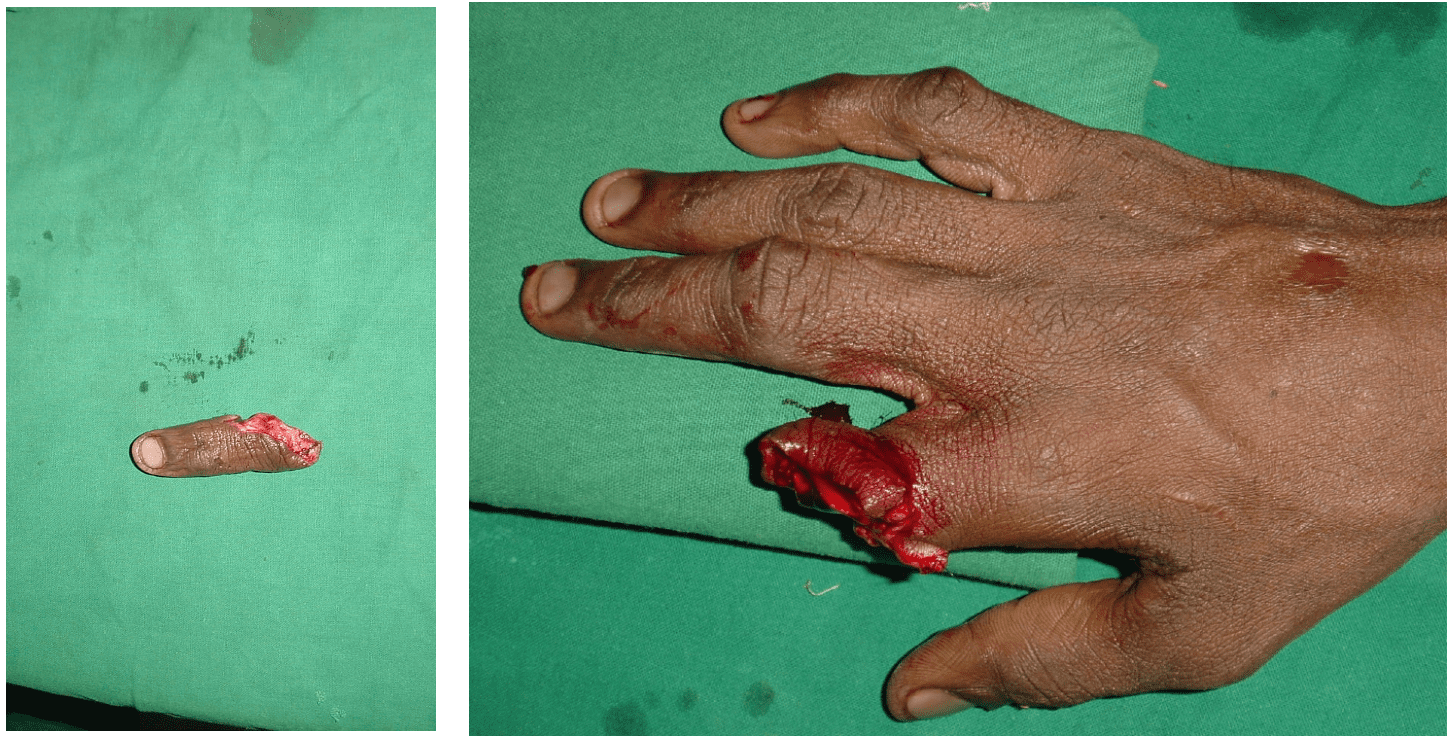

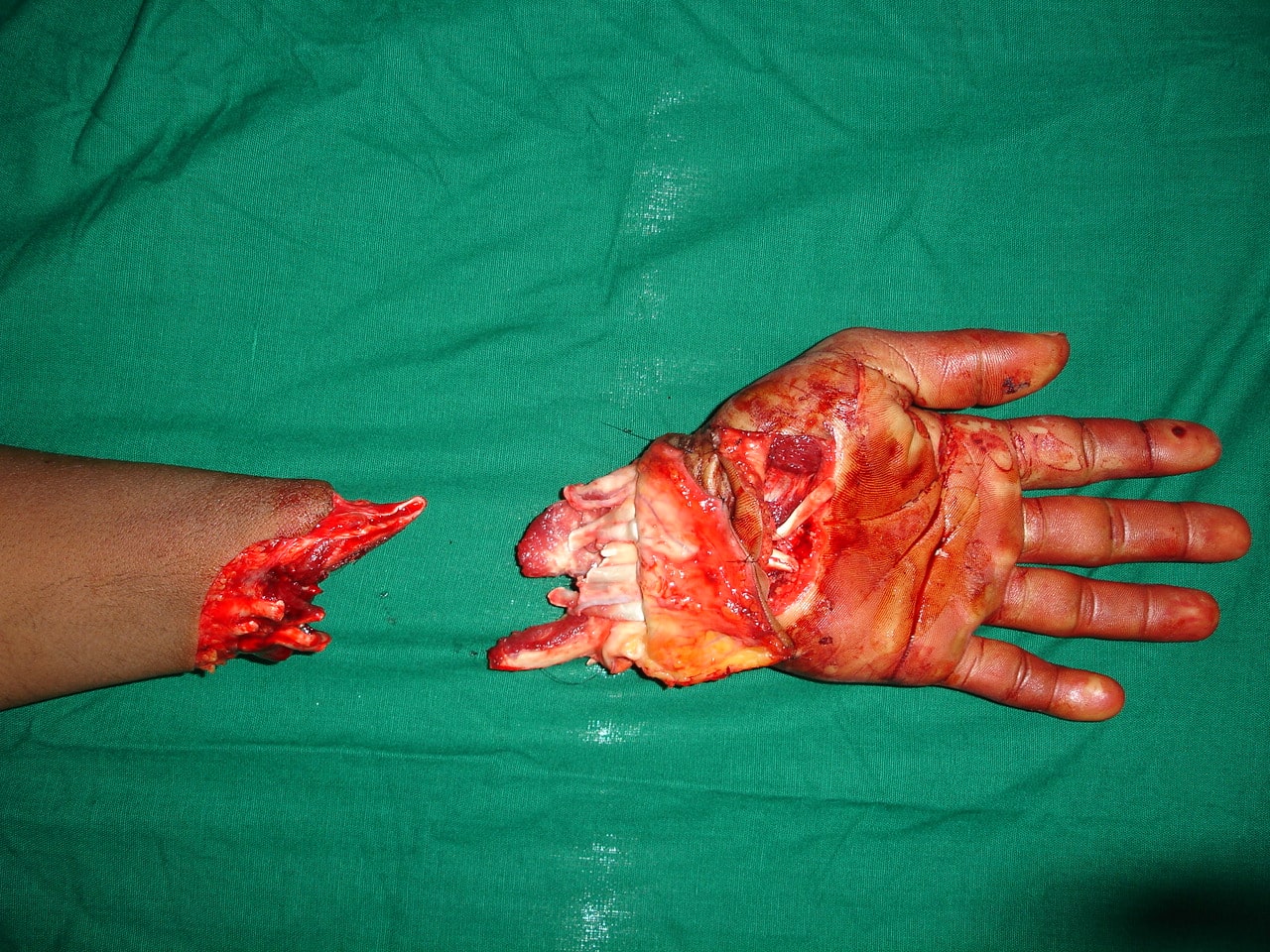







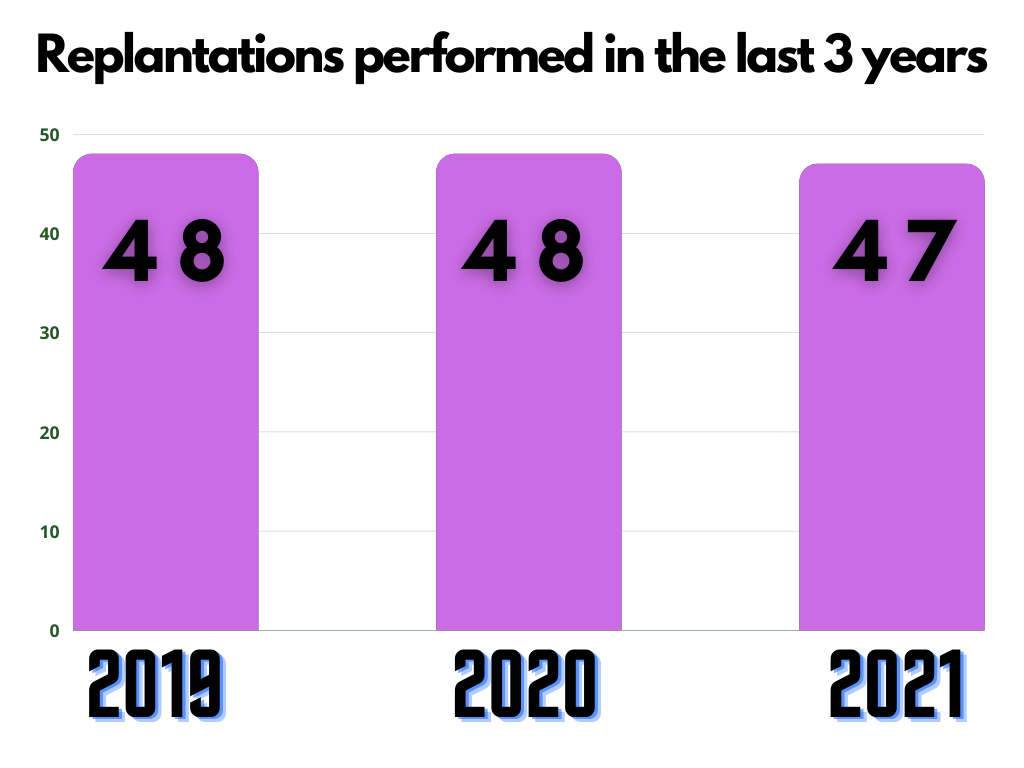
Replantation is the surgical process by which a completely cut off part of ones own body is reattached. This is not a mere stitching back of the severed part but is a complex procedure involving reconnecting cut bone, blood vessels, nerves and skin under magnification with delicate tissue handling.
Transplantation is a process by which tissue or an organ is transferred from one area of a person’s body to another area, or from one person (the donor) to another person (the recipient). This is entirely different from replantation which involved restoring a cut organ to its original anatomical position.
In some injuries it is seen that the injured part of the body does not entirely loose connection and may sometimes remain attached through varying amounts of tissue. Sometime despite injury to major blood vessels, these remaining connections may provide enough blood circulation to keep the partially amputated part alive.
However in most cases, these connection are merely flimsly strands of tissue or narrow bridges of skin that can not provide blood supply beyond the level of injury. In such circumstances the surgeon will require to repair the blood vessels providing and draining blood to the injured part in order to save it. This is known as revascularization and only differs slightly from replantation.
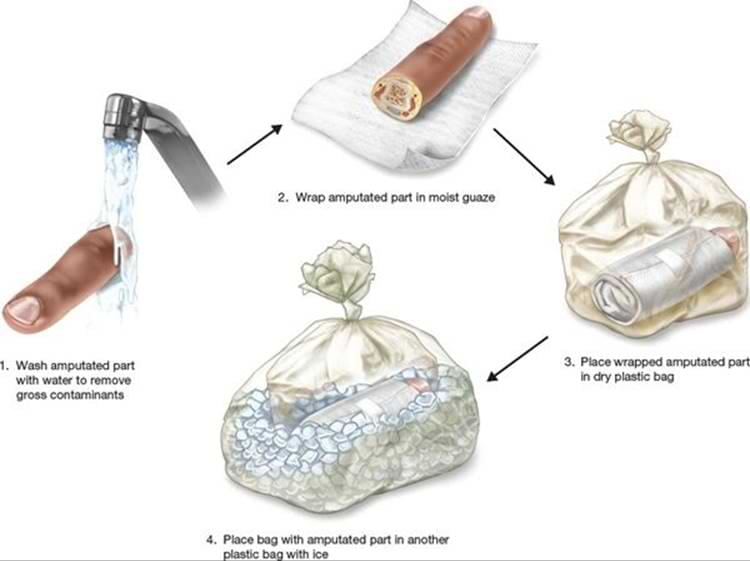
Theoretically Yes. But in practicality the suitability of a part that has been cut off to be reattached depends on mutiple factors and this decision should be made upon evaluation of an experienced microvascular surgeon. some of the factors that weigh in the judgement made by the surgeon can be time since the injury, state of the injured part, general condition of the patient after the injury, comorbidities and the amount of disability the patient may suffer due to loss of the part in question versus undergoing a complex reconstructive procedure. However it is the patients and by standers/ relatives duty to safely bring the cut part along with the patient to a hospital where adequate expertise is available for further opinion by a qualified surgeon.
The simple answer is immediately with no delay. But for the sake of stating scientific facts, with good technique of transport the chances for successful replantation/ revascularization of the severed part greatly increase if the patient reaches an operating room within 4 - 6 hours from the time of injury. This time can vary depending on the level of injury. For example the permissable time limit for an amputation at the level of the finger is more than that at the level of the arm.
This should be avoided as much as possible as in most injuries, blood can be controlled by pressure and elevation. In the event of rapid, uncontrolled bleeding, one may seek medical attention at the nearest health care facility but should inform the treating doctors that they intend to attain further management at an adequately equipped facility. The treating doctor will then be able to guide you, make arrangements necessary and in some cases even be able to communicate with the nearest specialist centre and inform them of your arrival. Common problems encountered with seeking local health care is when in an attempt to stop bleeding the vessels in the stump of the injured part are damaged, which makes replantation/ revascularization surgery difficult
Unfortunately No. After a successful procedure there may still be residual problems in the part such as stiffness, decreased sensitivity and functionality and raw areas which might require further surgical procedures. But with the combination of the right factors, surgical technique, good patient compliance and physiotherapy it is possible to achieve near normalcy in the damaged part.
With the advent of major advances in the field of prosthetics it is possible to provide some relief and independence to the patient. Prior to fitting of the prosthesis it is essential to achieve a stable and well healed stump at the site of injury.
Despite popular belief, even the most state of the art prosthesis have their own limitations. As per the principles of Reconstructive Surgery the best way to manage tissue loss in an injury is to replace "like with like". Even a stiff, non functional reattached part is almost always superior to the most advanced prosthesis that money can buy. Hence Replantation/ Revascularization must always be attempted when possible.