Specialization
- Brachial Plexus
- Breast Surgery & Reconstruction
- Burns
- Burns
- Cancer Reconstruction
- Cleft Lip and palate
- Congenital Hand Differences
- Cosmetic Surgery
- Diabetic Foot & Chronic Wounds
- Hand and Wrist Surgery
- Lower Limb Reconstruction
- Lymphedema
- Maxillofacial Surgery
- Microsurgery & Replantation
- Microsurgery Lab
- Skin Bank
- Spastic Hand
- Super Speciality Courses & Fellowships
Lymphedema
1. What is lymphoedema?
Lymphoedema is a swelling of a part of the body caused by an abnormal accumulation of lymph in the body.


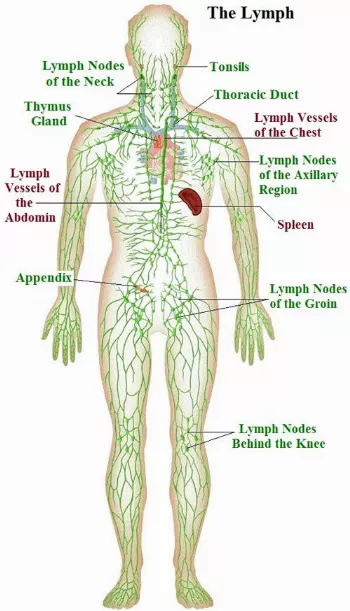
2. What is lymph?
At the level of the capillaries where there is an exchange of oxygen and nutrients to the cells, there arises a separate stream through which proteins, fat, fluid and white blood cells are carried. The fluid that passes through this is called as "lymph", and these separate streams are called "lymphatics".
3. Why does lymphoedema occur?
Lymphoedema occurs when there is a disturbance in the flow of lymphatics. Lymphoedema commonly occurs after surgical treatment for cancers such as breast cancer when a group of lymphatic tissue is removed, and the pathways to drain the lymphatics is affected.The chances of developing lymphoedema increases after radiotherapy. In India, lymphoedema occurs in patients affected with filariasis (Elephantiasis) where the lymphatic pathways are damaged. Rarely lymphoedema can also occur due to the paucity of lymphatic pathways by birth.




4. How does lymphoedema present?
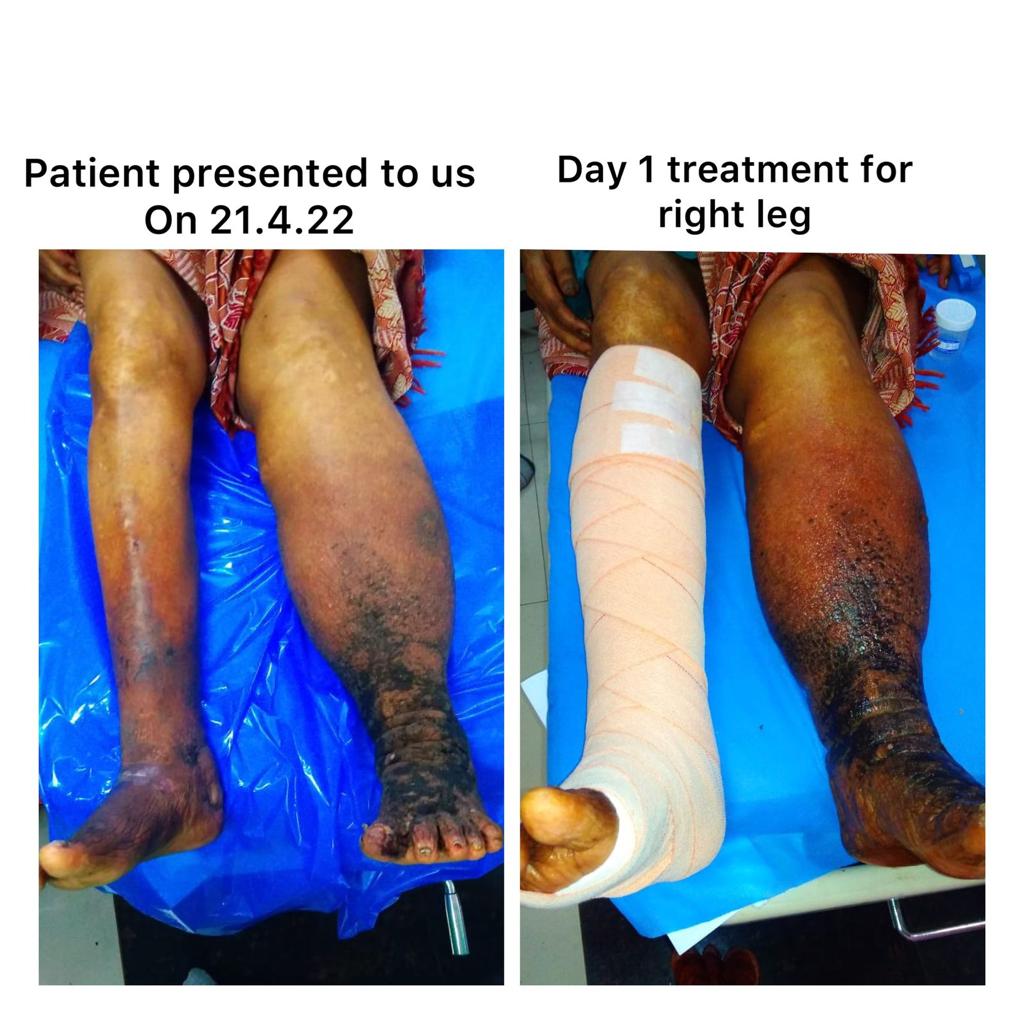
Lymphoedema presents as a chronically swollen limb which increases in size on keeping the limb dependent and reduces in size on elevating the limb and on compression. As the lymphoedema progresses, there could be difficulty in moving the fingers and toes, disabling a person to do work. The skin gets very thick with multiple warty projections, multiple folds and bulges. The patient may get ulcers which do not heal quickly. Patients with lymphoedema are very prone to develop an infection in the skin and subcutaneous tissue (cellulitis) and may develop a fever. With cellulitis, the affected skin appears swollen and red and is painful and warm to touch.

5. Is lymphoedema curable?
It is tough to cure lymphoedema. However, we can control lymphoedema. With treatment, patients feel better as they both look better and can improve the level of all activities done.
6. Is it too late to get treated?
Although we prefer seeing patients early, it is never too late to treat lymphoedema. For a motivated patient, it is never too late to improve the condition of the patient.
7. How can we prevent worsening of lymphoedema?
Worsening of lymphoedema can be done by getting lymphoedema treated at the appropriate time. Conservative management of lymphoedema is initially done, and the patient is evaluated and accordingly, the treatment plan is decided as per each patient.
8. Can lymphoedema be managed without an operation?
All lymphoedema patients are treated initially without operation for atleast 6 weeks. The patient is instructed to have strict bed rest and elevate the limb. We allow the patient to move around only for going to the toilet. Four-layer compression bandages and lymphatic pumps are applied to reduce oedema. Skincare is given in the form of moisturising creams. Physiotherapy in the form of exercises to move the toes and fingers and manual lymphatic drainage is taught to the patients and the attenders which help in reducing the lymphoedema.





9. How is lymphoedema evaluated?
When a patient with lymphoedema comes to our hospital, we get a detailed history regarding the swelling and treatment, examine the patient, take photos of the limb and evaluate the size of the limb using specific formulas. Some patients may have some co-existing venous abnormalities, and a scan is done for the same. If the patient also has varicose veins due to incompetent perforators, treatment of the varicose veins may help reduce the limb swelling to a considerable extent and is done before any treatment for the lymphoedema.
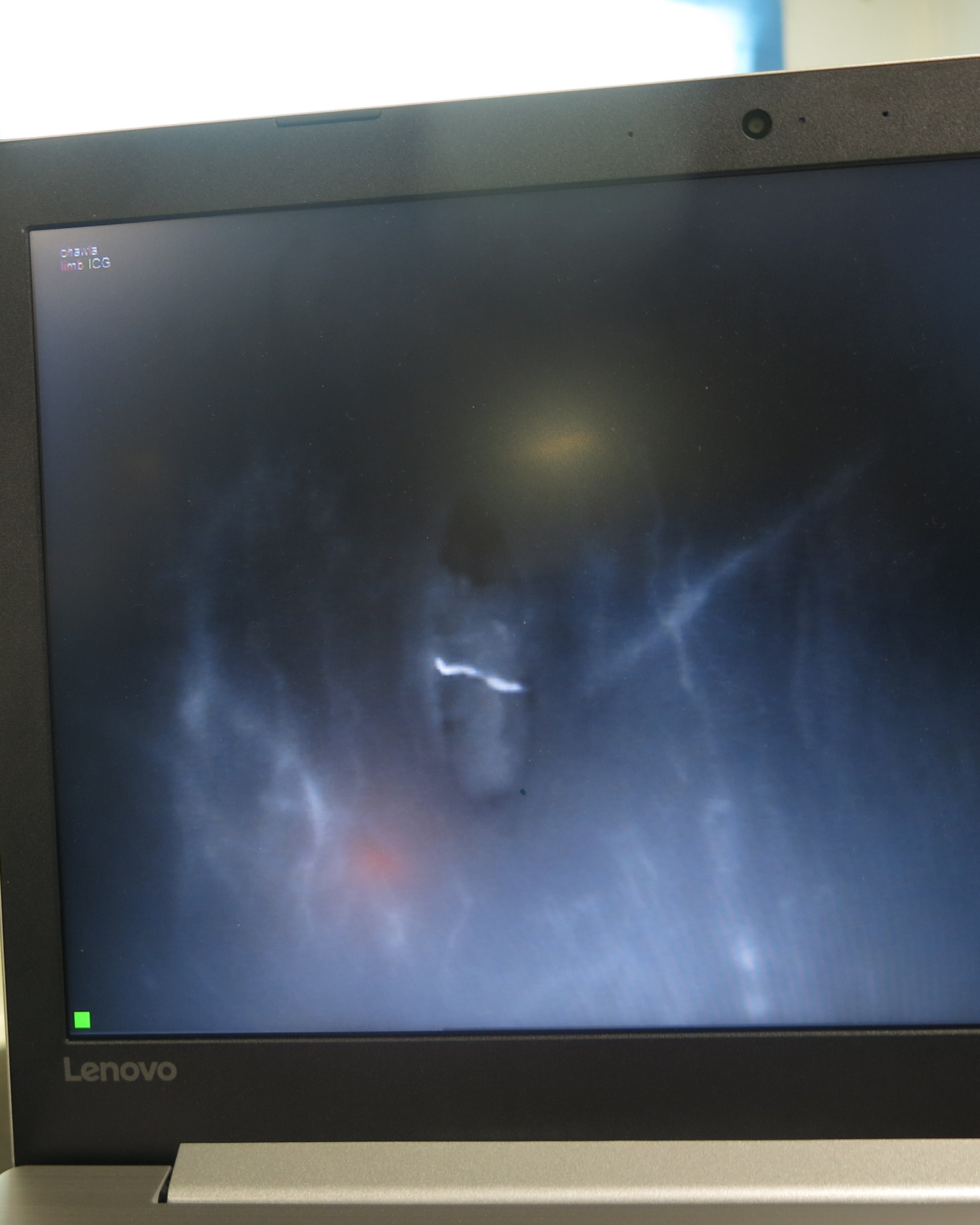
We then evaluate the condition of the lymphatics by doing an ICG (Indocyanine Green) lymphangiography. Indocyanine green is a water-soluble drug containing iodine which has been safely used by eye doctors for several years to look at the condition of the vessels in the eyes. ICG (Indocyanine green) is injected into the skin of the patient mostly between the toes or the fingers and is taken up by the lymphatic vessels. When LASER light is shown on the part containing the ICG, the molecules get excited and emit infrared rays which are captured by a camera and shown on the screen. The ICG lymphangiography identifies the position of the lymphatics, evaluates the condition of the lymphatic vessels, the level of obstruction in the flow of lymphatics and the speed with which the ICG moves in the lymphatics is found out by the scan. The scan can take about 20 to 30 minutes. The patient is also able to visualise the condition of his/her lymphatics, and we explain to the patient in detail about the problem, the condition of the lymphatics. We then discuss and formulate a surgical plan for the patient.
10. How is lymphoedema treated surgically?
The surgical treatment of lymphoedema can be broadly divided into physiological procedures wherein an alternate pathway to divert the lymphatic tissue is formed from the obstructed lymphatic system to the venous system or debulking procedures where the excess tissue is removed. Physiological procedures include Lymphovenous Anastomosis (LVA) and Vascularised Lymph Node Transfer (VLNT) and debulking procedures include Surgical debulking and liposuction.
11. How and when is Lymphovenous Anastomosis(LVA) done?
Lymphovenous Anastomosis (LVA) is done by connecting lymphatic vessels lesser than 0.8 mm to small veins using microsurgery to form an alternative pathway to drain the excess lymphatics. LVA is done in only in early stages where there are good functional lymphatics. We decide to LVA only when we see a linear pattern in the ICG lymphangiography. We are also able to find out the exact position of the small lymphatics and see whether the LVA is patent by using ICG lymphangiography.



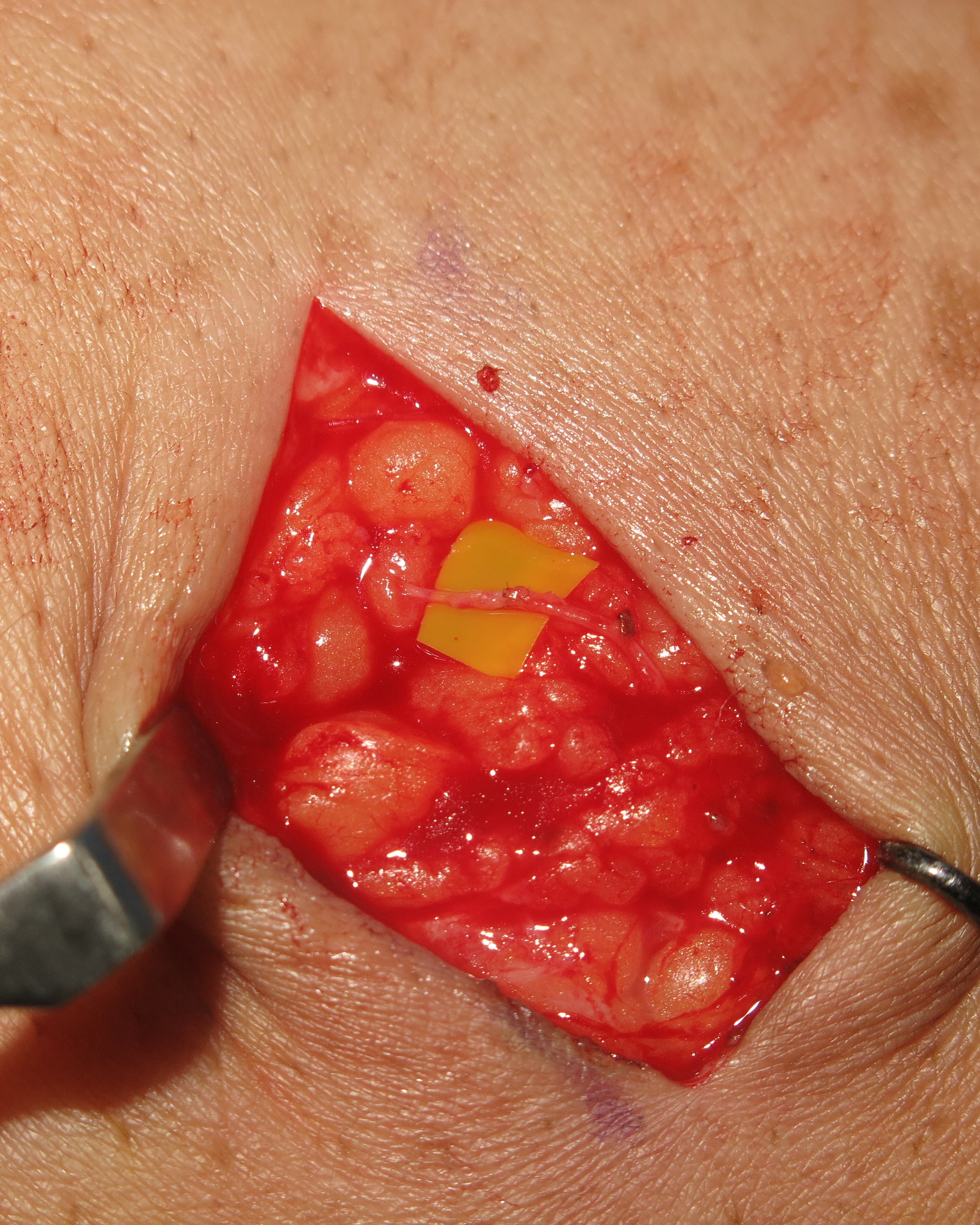



12. How are patients with LVA managed post-operatively?
As the incisions are only skin deep, there isn't much pain for the patient, and the patient can be discharged within three days. Compression bandages are applied post-operatively. Reduction in the size of the limb is usually evident within 2 days. However, to obtain the best results, we advise the patients to apply compression garments throughout life.
Facts at a glance about Lymphovenous Anastomosis (LVA)
· Number of days stay in hospital : 3 days
· Resumption of Walking : 1 week
13. How and when is Vascularised Lymph Node Transfer (VLNT) done?
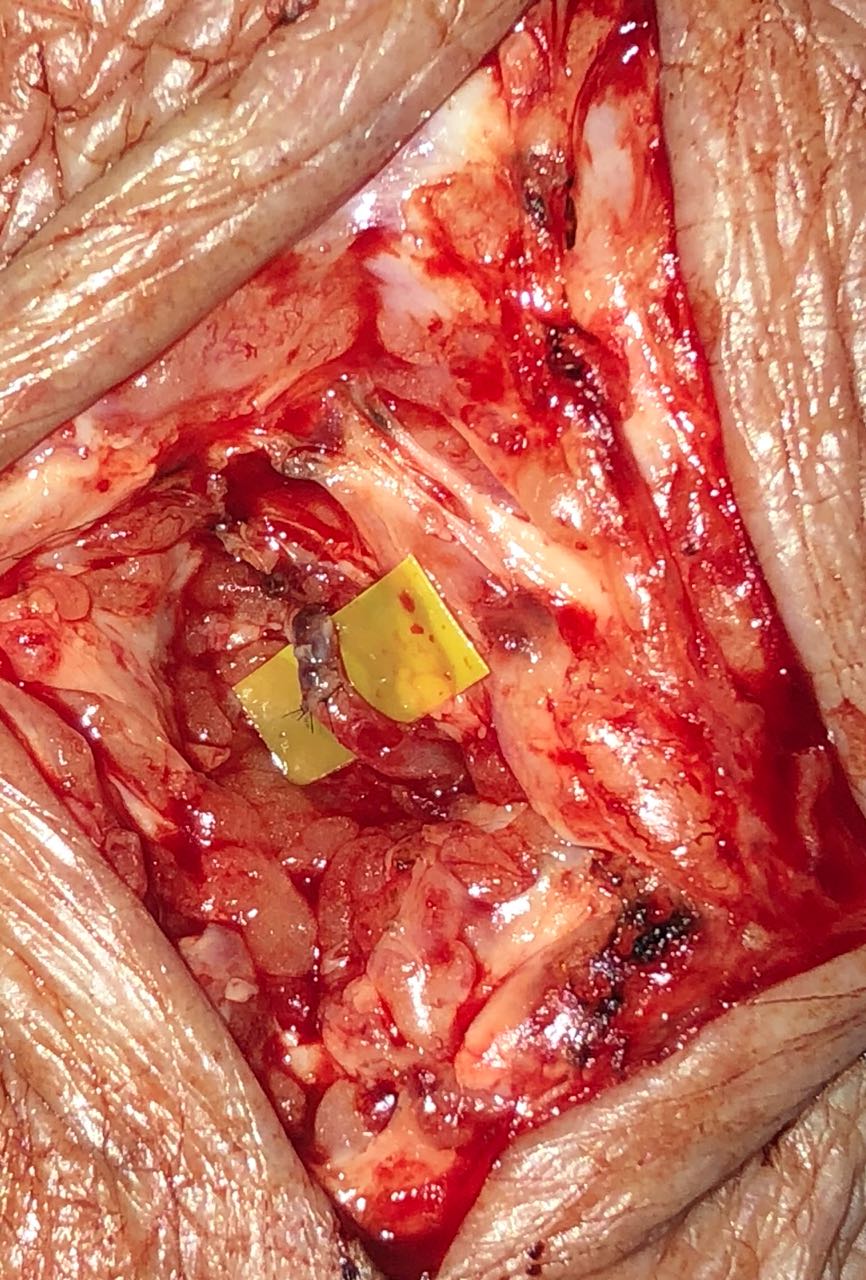
Vascularised Lymph Node Transfer (VLNT) is done using microsurgery to replenish missing lymph nodes in the affected extremity by transferring healthy lymph nodes from another region to the affected area. VLNT can be done both in the early stage as well as in the late stages. Vascularised lymph node transfers are also done along with LVA in certain conditions to get better results. Patients with breast cancer developing lymphoedema can be treated effectively by breast reconstruction using the excess skin and fat below the umbilicus, which is taken along with the lymph nodes and transferred to the chest. The advantage of this procedure is that in addition to reducing the size of the affected limb, the breast is also reconstructed at the same time to give a better look. Otherwise, tissue containing lymph nodes from the neck, axilla or the abdomen is used for the transfer to the affected limb with lymphoedema.









14. How are patients with VLNT managed post-operatively?
Since Vascularised lymph node transfers involve microsurgery wherein blood vessels of size 1 to 2 mm is connected, the viability of the flap and the patency of the anastomosis is frequently checked every 2 hours by trained nurses in a special Microsurgical post-operative room. After 5 days, the patient is transferred to the room, and the patient can be discharged within 10 days from surgery. We would then apply compression garments to make the limb smaller.
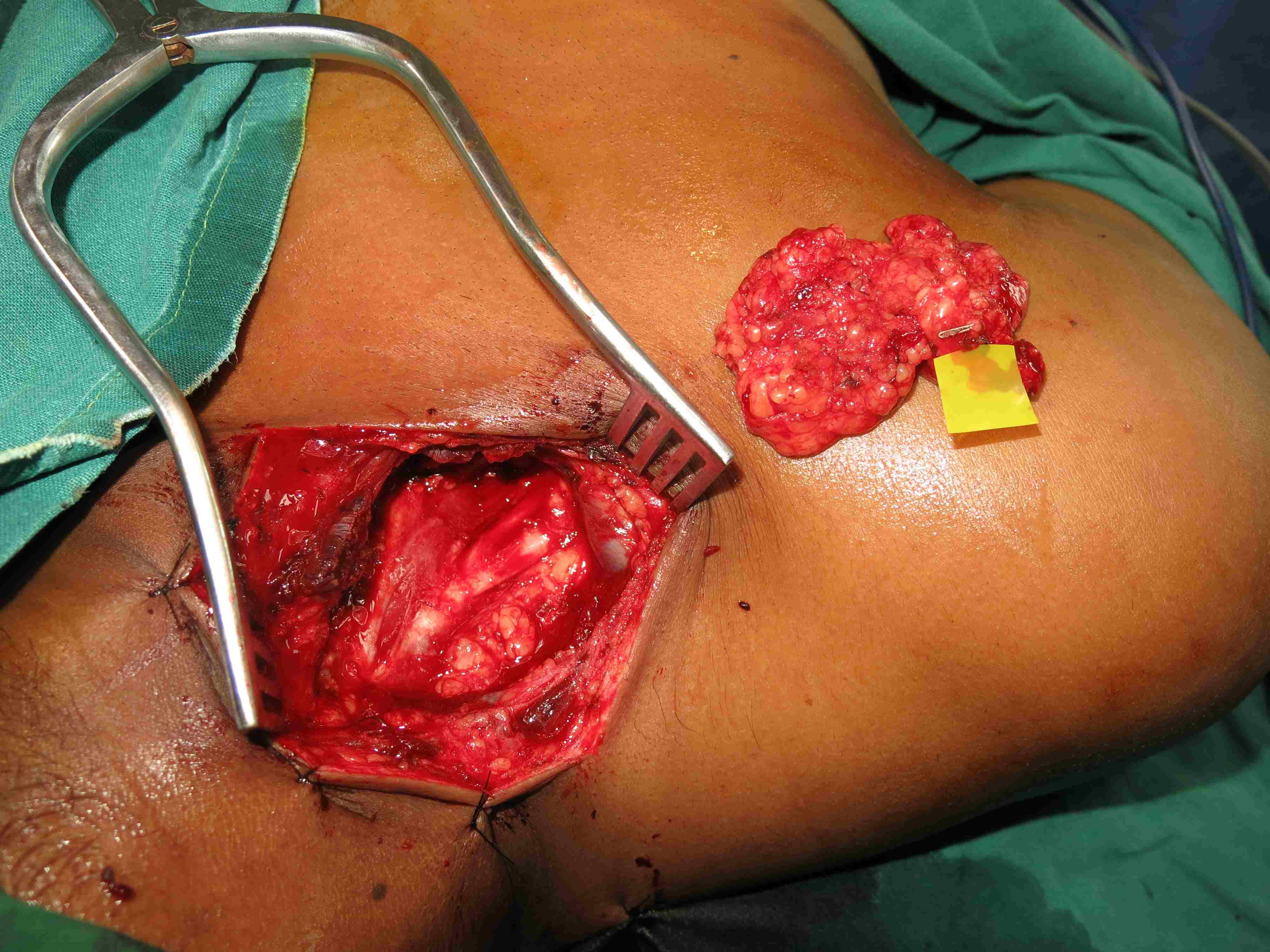
15. How and when is surgical debulking done?
Surgical debulking is done in advanced cases where there are skin changes and in most cases of filariasis. In this the excess skin, subcutaneous tissue and fascia are removed. The defect can then be either closed primarily or covered with split skin grafts to make the wounds heal well.







16. How are patients for whom surgical debulking was done managed post-operatively?
After the operation, compression bandages are applied, and the limb is kept elevated to reduce oedema. Dressings are commonly done in the 3rd and 5thday. Patients are commonly discharged within 5 to 7 days. The patient is asked to come after 2 weeks to remove the sutures. If grafts are applied, they may need dressing changes every 5 to 7 days until the wounds heal. The wounds are expected to heal within six weeks after grafting.


17. How and when is liposuction done?
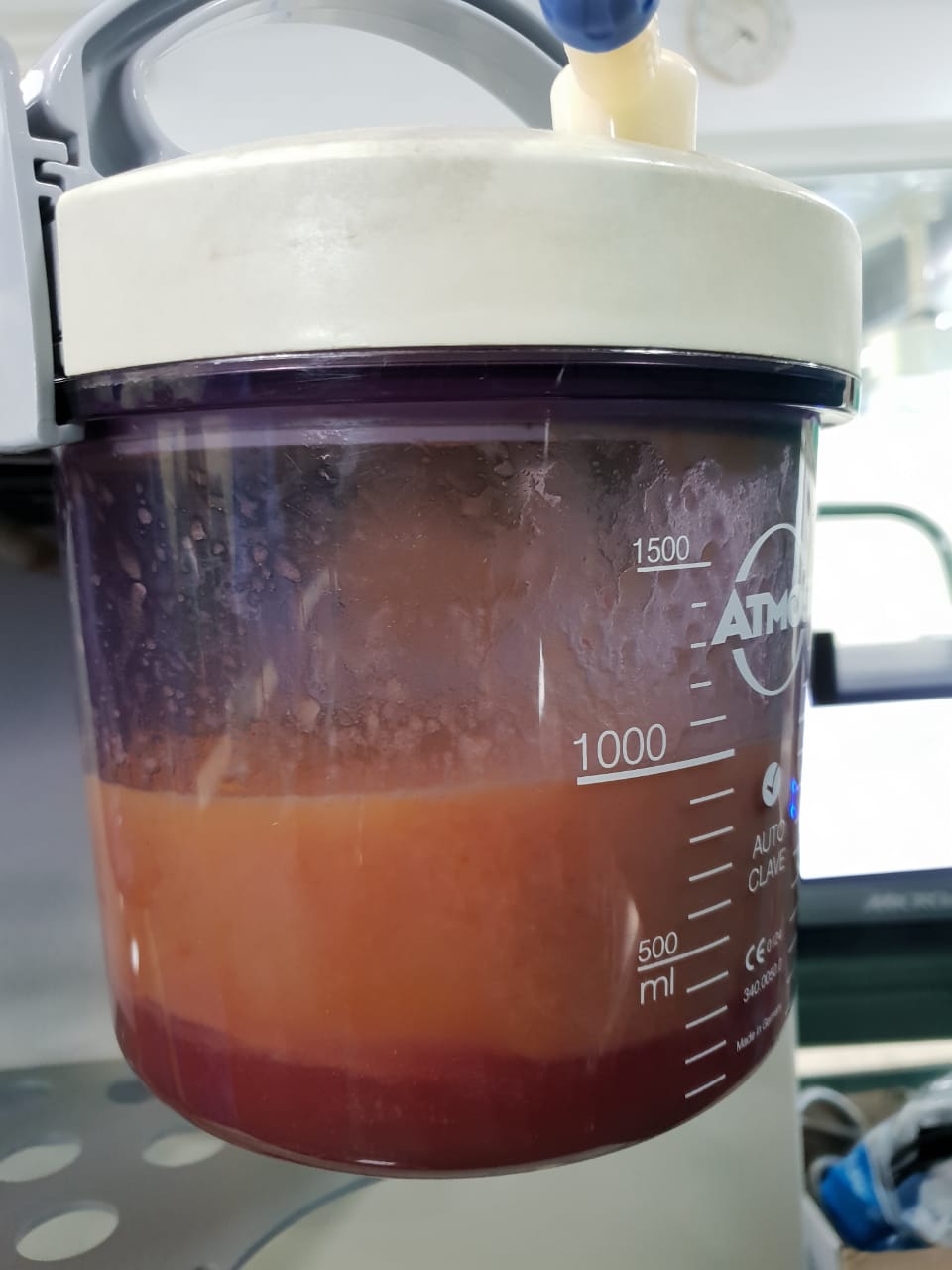
When there is an obstruction to the drainage of lymphatic fluid, there can be excessive growth of fat in the tissues. After the abnormal lymphatic collection in lymphoedema has been treated by physiological procedures such as Vascularised lymph node transfers, Lymphovenous anastomosis and even conservative methods, the excess fat in the limb is treated by liposuction. Small stab incisions are made, liposuction cannulas are inserted, and the excess fat is sucked out.
18. How are patients for whom liposuction was done managed post-operatively?
After liposuction, the limb is wrapped with compression bandages and is kept elevated. The patient is advised to move the toes and fingers. Most of the stab incisions would heal by itself and rarely may need removal of sutures if they were placed earlier. The patient may need to stay in the hospital for 2 to3 days. We then advise the patient to wear compression garments throughout the life as best results are got after that.
19. Some DO's and DON'T's for patients with lymphoedema
Dos
1. Keep the skin meticulously clean and frequently check for any cracks, fungal infections or rashes
2. Use a moisturising soap to take a shower or a bath.
3. Dry the skin especially the gap between the toes thoroughly with a soft towel after taking a bath
4. Elevate the lymphoedematous leg as much as possible
5. Wear the compression stockings or garments given throughout the day.
6. Exercise as much as possible as discussed with the physiotherapist.
7. To visit the doctor if there is increasing pain, redness and fever
DONT's
1. Avoid tight clothing such as a tight blouse, undergarments or socks
2. Do not walk barefoot, especially in temples under the hot sun.
3. Avoid wearing bangles, watches and rings in the limb affected with lymphoedema.
4. Keep the nails short. In the same time avoid having very short nails.
5. Try to avoid injections in the limb affected with lymphoedema
6. No piercing or tattoos in the limb with lymphoedema
7. Avoid adding weight. It makes the lymphoedema worse.
8. Avoid hot showers.
20. How is Ganga Hospital unique in the treatment for lymphoedema?
· Lymphoedema involves a holistic approach in the treatment for lymphoedema and needs a team of experienced surgeons, physiotherapists, nurses, dieticians trained in lymphoedema.
· The appropriate evaluation of lymphoedema is critical to know how to decide upon the treatment for lymphoedema. We are one among the very few centres in the country who evaluate all lymphoedema patients with ICG lymphangiography. ICG lymphangiography not only helps us in understanding the problem and deciding the treatment, but it also helps the patient and his/her family to understand the problem that they are facing.
· Ganga Hospital is unique in that it is capable of doing and has done all procedures acceptable for lymphoedema such as Vascularised Lymph Node Transfer(VLNT), Lympho venous Anastomosis(LVA), liposuction and surgical debulking. As we are capable of doing all procedures, we do the procedure that we feel is the best suited for the patient.
· Procedures such as Vascularised Lymph Node Transfers(VLNT) and Lympho Venous Anastomosis (LVA) need a very experienced team of plastic surgeons trained and specialised in microsurgery as they may involve suturing lymphatic vessels less than 0.8 mm
· Liposuction in a limb with lymphoedema needs "Power Assisted Liposuction" as fat needs to be sucked in very fibrous areas. We are proud to have this in our armamentarium
· Ganga Hospital has always been a very patient-centric hospital. It has grown from humble beginnings to this extent as we have always believed that the patient's interest and well being is our only interest.
Surgeons
Events
Research
Vascularized Lymph Node Transfer From Thoracodorsal Axis for Congenital and Post Filarial Lymphedema of the Lower Limb
Vascularized lymph node transfer is becoming a popular method to treat lymphedema. We have performed vascularized lymph node transfer for two patients, one with congenital and the other with post filarial lymphedema of the lower limb