Specialization
- Brachial Plexus
- Breast Surgery & Reconstruction
- Burns
- Burns
- Cancer Reconstruction
- Cleft Lip and palate
- Congenital Hand Differences
- Cosmetic Surgery
- Diabetic Foot & Chronic Wounds
- Hand and Wrist Surgery
- Lower Limb Reconstruction
- Lymphedema
- Maxillofacial Surgery
- Microsurgery & Replantation
- Microsurgery Lab
- Skin Bank
- Spastic Hand
- Super Speciality Courses & Fellowships
Maxillofacial Surgery
The unit of maxillofacial surgery is a part of the Department of Plastic and Reconstructive Surgery dealing with the management of facial trauma, congenital and acquired deformities of the head and neck, diseases like infections, cysts and tumours of the teeth, upper and lower jaw and Temporomandibular joint-related disorders. Most of the problems require a multidisciplinary approach and plastic surgeons, maxillofacial surgeons and neurosurgeons working together has helped us provide wholesome care to the patient.
1. Maxillofacial Trauma
In India, the major cause of facial injuries is associated with road traffic accidents. The severity depends on the velocity of the trauma and protection at the time of injury. Wearing helmets while riding a 2-wheeler and seat belt when driving a 4-wheeler helps reduce the severity of trauma to the face.
The type of injury varies from simple lacerations to multiple facial bone fractures. These can also be associated with injuries to other areas of the body. The treatment will depend on the type of injury sustained.
It can vary from small cut wounds to big abrasive wounds and degloving wounds. The primary aim is to clean the wound thoroughly and help heal with minimal scarring. The surgical procedure will vary according to the type of wound and amount of soft tissue loss. Simple cut wounds can be sutured whereas bigger wounds will require skin graft or flap surgery to aid in healing.
Does a small cut would which is less than a centimeter needs to be stitched?
A deep small cut needs to be sutured as it will help to minimize the scar.
Do I need to stay in the hospital?
If the procedure is done only under local anesthaesia then the patient can go home after the operation Bigger wounds which are bleeding profusely or multiple wounds that need to be cleaned and stitched may require general anaesthesia. In some cases where there is tissue loss, a skin graft or flap surgery may be done to close the wound. In such instances the patient will need to be admitted in the hospital.
How to take care of the wound?
If there is no dressing, the patient can start to wash his face regularly with facewash and then apply antiseptic ointment. This will help to keep the wound clean and prevent any infection. The sutures then are removed after a week. In case of skin grafting the patient will have a dressing for 2 weeks. Patient can start to wash the face after the dressing is removed.
Treatment of scars
The patient initiates scar massage about a week after the stitches are removed. The process of massaging the scar is taught to the patient who will do it for about a year. Sometimes a little extra help may be required to settle scars. This involves the use of pressure garments and silicone gel sheet application.
Will I need a second surgery?
This will depend on the scar healing. Scar massage needs to be done for a minimum of 6 months to soften the scar and prior to deciding on the need for a correction surgery. There are chances for the scar to become big or distort the facial structures, we can correct them with flaps or fat grafting.
Will the lost hair lost on the mustache and eyebrow regrow?
Hair does not regrow on the scar line. However once healing occurs hair growth in the adjacent area may mask the scar. If required a procedure called Hair Transplant maybe done to help cover the scar.
Normal anatomy of a tooth and its supporting structures
The part of the tooth that can be seen in the mouth is called the crown and the part that is within the bone (alveolar socket) is called the root.
The tooth is held within the bone by means of supporting ligaments called periodontal ligaments.
The tooth has blood vessels and nerves within the pulp chamber and the canals making it a viable structure.
The injuries to the tooth can be
Dentoalveolar fractures - Fractures of parts of the tooth and its underlying bone.
Concussions – blunt injury to the tooth.
Luxations- When the tooth has lost its support and is moving within the socket.
Intrusion and extrusion -where it is pushed into or partially out of the socket.
Avulsions – When the whole tooth is lost and completely out of the socket.
Can an avulsed tooth (tooth that has come out of the bone and is without a fracture) be replanted back in the socket?
Only the permanent tooth can be replanted back in the socket and not the primary (baby) tooth. The criteria for good outcome following replantation of a completely avulsed tooth are:
The tooth should be brought in a proper manner (as described below) to the doctor within an hour after it has fallen out so that he can successfully place the tooth back in its socket.
There should be no associated root fractures.
The supporting periodontal ligament (supporting ligament present on the surface of the root of the tooth) should be viable at the time of replantation
The tooth once replanted should be kept immobile for a period of 8 weeks by means of splinting.
How to get an avulsed tooth to the hospital?
The tooth needs to be washed in running water to remove off the dirt. Make sure that you do not scrub the surface of the root as it will remove off the periodontal ligament attachment of the tooth.
The tooth needs to be kept moist and the best way to do that is to gently put the tooth back in the bony socket from where it was lost. You can also place it in a container filled with milk or tender coconut water.
Once you arrive at the hospital the doctor will assess the condition of the tooth and if found good, the doctor can reposition and stabilize it by taking support from the adjacent good teeth by means of splinting (using wire, clips or cement).
Dentoalveolar fractures
These fractures involve the bone supporting the teeth. When such a fracture happens, the patient will have bleeding from the mouth and the involved teeth will be shaking. There may also be some cuts and bruises in the oral cavity.
Can the teeth be saved?
The fracture can either be splinted (arch bar and /or stainless-steel wires will help support the tooth) or fixed with titanium plates and screws depending on the size of the bony fracture and number of teeth involved. If the tooth is in a bad shape, then it cannot be retained and must be removed.
How long will the splinting be in place?
The arch bar and wires will be retained for a period of 6 to 8 weeks. Once the teeth are firm the arch bar and wires will be removed in the outpatient department. This will be followed up with a dental Xray and RCT (root canal treatment) for the involved teeth.
What can I eat during the time that my teeth are splinted?
It will best be to have a liquid or semisolid diet to avoid putting any pressure on the teeth till they heal. No chewing allowed for 6 -8 weeks!
When can I suspect that my jaw is fractured?
When the upper jaw (maxilla) or the lower jaw (mandible) is fractured you will notice that your teeth do not contact well, face appears swollen or deformed and you have difficulty opening the mouth. You will also experience pain when chewing on food. There may be bleeding from your mouth and hematomas in the cheek, floor of the mouth or in the palate. Some teeth may be lost or mobile.
Do I need surgery?
Surgery needs to be done for most of the fractures of the jaw. It will be done under general anesthesia and the fractures will be fixed using titanium plates and screws (ORIF – Open reduction and internal fixation). In some cases, the fractures are not very much displaced and in this situation they can either be managed without any surgery or by means of intermaxillary fixation (wiring the teeth together).
What is intermaxillary fixation
Intermaxillary fixation is basically wiring up the upper and lower jaws together such that you cannot open your mouth. It will be retained for a minimum of 2 to 6 weeks depending on the location of the fracture and how much it affects the way your teeth occlude. During this period, you need to be on a liquid diet. You can keep your oral cavity clean by regular brushing and gargling with a germicidal mouth rinse. Once the wired jaws are released, you need to do rigorous mouth opening exercises to improve the mouth opening. You can also start having solid foods and maintain better oral hygiene.
What do I need to do when my fractures are fixed?
If the fractures are fixed you need to be on a semisolid diet followed by soft diet for a period of 6 weeks after which you can resume a normal diet based on how the healing has taken place. Sometimes even if the fracture is fixed the jaws can be wired. This is done especially when there is more than one fracture or if it is comminuted (broken into many bits.) In that case you need to follow the instructions as for intermaxillary fixation. It is important that you maintain good oral hygiene by regular brushing and rinsing as there will be stitches inside your mouth which can get infected.
Do I need to remove the implants after recovery?
Usually, titanium plates need not be removed. There is more than 90% success rate. If there is infection following surgery, plates and screws may be removed only after a minimum of a year’s time. Till then we will be treating him with medications.
What are the expected complications following surgery?
Infection at surgical site, nonunion of the bone, wrong union (malunion) of the bone, numbness over lip or cheek depending on the fracture. All these are treatable. Numbness usually settles over a period while infection is treated with medicines. In case of nonunion or wrong union, further surgery may be needed to correct the problem.
Cheek bone fracture also referred to as zygomatic complex fracture. This fracture presents with redness of the eye and bruising of the eyelids, flattening of the cheek on the involved side and numbness of the cheek, upper lip and teeth of that side. Patient can also experience pain and restriction while opening the mouth and chewing food. Sometimes the vison in the same side eye can also be affected. Immediately after the injury there can also bleeding from the nose and mouth. This fracture can also occur along with fracture of the upper jaw in which case the patient will have disturbance in his bite.
What is the treatment?
Grossly displaced fractures need treatment as there will be severe restriction in opening the mouth and flattening of the cheek. The procedure is done under general anesthesia. Most of the accesses to this fracture will not cause any scarring on the face. Depending on the need, the fracture will be fixed with plates and screws.
What are the precautions that I need to take following surgery?
The following set of instructions will be given to the patient prior to discharge following surgery for correction of cheek bone fracture
While sleeping the patient needs to keep the head end elevated and not apply any pressure on the surgical side. This needs to be followed for a period of 6 weeks till the bone heals.
Patients are instructed to take soft diet and follow good oral hygiene measures even if they have stitches place inside the mouth. Normal diet can be resumed 6 weeks later.
Patient can also take a bath everyday even when there are stitches in the scalp. Keeping the surgical site clean is of utmost importance to avoid infection.
Mouth opening exercises are taught to the patient on their first follow up. Doing the exercises regularly and as instructed will help improve the mouth opening to the preinjury mouth opening.
Will the sensations over the cheek, nose, lips and teeth return?
The numbness is caused because the sensory nerve is crushed when the bone is fractured. In most of the cases the sensation returns back in varying intervals between three months to 2 years.
2. Jaw cyst and tumors
Jaw cyst and tumors are the swellings that occur inside or over the jaw and face .Mostly they are non cancerous (benign) but it still can cause massive invasion affecting nearly half of a jaw or entire jaw.
Some of them show swelling noticeably but some of the cyst and tumor can behave silent too .On a regular dental visit the cyst might be revealed!!
The most common affected area is the third molar region or the wisdom tooth region in the lower jaw which usually is not fully erupted or not at all erupted ,followed by canine region and then in upper jaw .
What causes the cyst and tumor in jaw bones ?
Usually these cyst and tumors originate from the tooth forming cells. Usually these cyst and tumors are detected in the 2-3 decade of life .
There can be cyst and tumors without odontogenic origin .they are usually associated with some other syndromes like Gorlin Goltz syndrome etc.
Signs and symptoms :
Swelling over face usually lower one third of face
Loose tooth
Painful mouth opening
Bad taste
Malpositioning tooth (originally placed right )
Fracture of jaw
What will be done at the hospital ?
Initially a thorough evaluation will be done and a set of radiographs including an orthopantamogram or a paranasal view will be done according to the suspected area of swelling .we might need a computed tomogram (CT) for clearer details.
After the radiographic evaluation is done we will be able to come to have an idea what is the condition .to confirm a biopsy will be taken . After we receive the biopsy report a final treatment plan will be made.
Treatment options :
Surgical options
Removal of the cyst in one piece-if it is small in size
Removal of the cyst over a period of time -if it is too big we allow it to shrink and then remove on the whole .
Removal +Reconstruction :
Here we remove the tumor on the whole which usually may be half of the lower or upper jaw . Following removal of the jaw the patients may not be able to chew food or have difficulty hence we have reconstruction options to aid in bringing back the patients life to near normal.
We can reconstruct the jaw with bones from the leg. After a thorough evaluation a portion of the bone from the calf region is taken along with its blood supply. This bone is cut into shape of the jaw bone and fixed there with plates and screws. Then the blood vessels from the remodified jaw(leg bone) is connected with the blood vessels of face. This surgery is performed under general anaesthesia and a minimum of 3 weeks stay is needed .Following this lost teeth can also be replaced with dental implants over a period of time .

JAW CYST AND TUMOUR
3. Temporomandibular Disorders
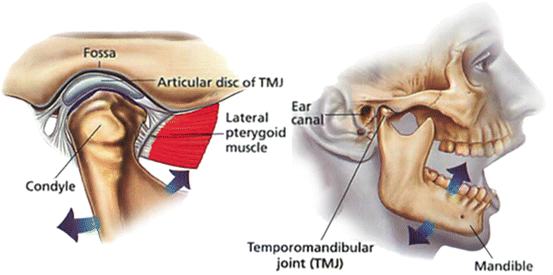
The temporomandibular joints (TMJ) are the joints that connects the lower jaw and skull. This joint helps us in opening and closing the mouth .In this joint there are few ligaments,muscles,discs apart from bones. If this entire unit functions in one piece then there no trouble .But when there is a non synchronized function there might be a temporomandibular dysfunction/disorder.(TMD).
Are there any specific reasons for TMD?
In most of the cases there are no particular causes for this condition .But most of the time its due to wrong positioning of jaw ,continuous grinding of teeth,some habits like biting nails or opening bottles in front teeth .In all these actions unknowingly the affected person gets his lower jaw in front ,which is ideally a wrong position for the jaw (i.e) the jaw is stretched to a forward position . Over time there is disturbances like disc displacement ,bony resorptions etc. These are believed to be the causes and reasons behind TMD.
How do I know if I have TMD ?
Most common features that an affected person might have :
Swelling over face usually lower one third of face
Pain in front of the ear
Difficulty to open mouth widely
Some clicking or grating sounds while opening or closing the jaws
Headaches - can spread to neck and back
Inability to close jaws
Restricted movements of jaw
These symptoms can be a differential diagnosis for many other conditions. it is better to consult with the doctor if it is persistent.
What are the treatment option for this condition ?
It is based on various aspects. It is not the same for every individual.It varies from person to person ,at what stage he /she comes to us ,is he having any other correlating conditions like rheumatoid arthritis , is there any emotional disturbances or stress.
These patients can fall into two categories for treatment
1. Conservative/medical therapy
2. Surgical therapy.
Conservative therapy includes the patients with mild symptoms which can be corrected with stopping the habit like night grinding of teeth or biting nails ,etc.some of the might need relaxation therapy where they will go through stress management , meditation .Mostly a soft bland diet is advised. Jaw strengthening exercises are taught to relieve the stress .Hot /cold water fermentation is also relieving!!ed jaw(leg bone) is connected with the blood vessels of face. This surgery is performed under general anaesthesia and a minimum of 3 weeks stay is needed .Following this lost teeth can also be replaced with dental implants over a period of time
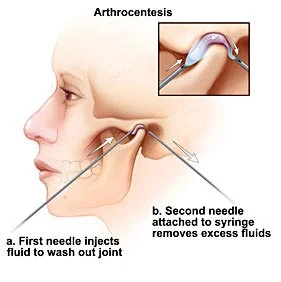
Surgical treatment like arthrocentesis ,arthroscopy, disc plication ,eminectomy, condylectomy ,discectomy ,joint replacement are available.
Arthrocentesis is a simple day care procedure wherein two needles are inserted into the joint space and flushed with sterile fluids and medicaments to lyse the adhesions . Through one needle the fluids are flushed in under pressure the fluid along with adhesions are flushed out through the other needle .
Arthroscopy is a procedure where the joint is viewed through a camera inserted through the key hole made . Procedures can be done through arthroscopy like plication or cuttuing or even flushing out the joint .This procedure will need general anaesthesia and a few days of stay in hospital .
Disc plication is a procedure where the disc of the joint is exposed under general anesthesia. In some conditions the disc might get displaced to a wrong and unfavorable place .The corrective procedure is to get back the disc and to tighten the ligaments to help stay in the preferred zone .
In case of recurrent dislocations we might proceed with a procedure called eminectomy where the articular eminence of the bone is cut and removed to enhance the free movement of the condylar head .This is also done under general anaesthesia .
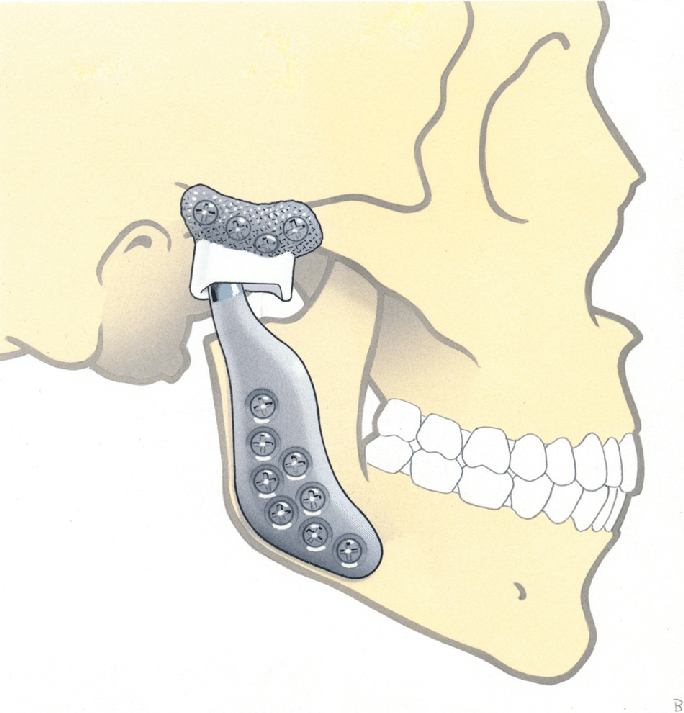
Condylectomy is done in cases with degenerative diseases of the joint ,recurrent dislocations or lock jaw ,ankylosis where the can be bony or fibrous adhesions around the joint not allowing movement to happen .Here the condyle is removed either partially or in toto.
Joint replacement is a procedure where the entire joint is replaced with two components including the cranial component and the lower jaw component .This allows free movement of the joint enhancing mouth opening and chewing .This treatment is done in cases of severe ankylosis.
4. Dental Support
Oral health care as well as smile designing is done in our dental division. Oral health maintenance and smile designing needs the interaction of various dental disciplines like orthodontics, prosthodontics, periodontics, conservative dentistry and oral and maxillofacial surgery.
Orthodontics
What is orthodontic Treatment ?
Orthodontics is the branch of dentistry that corrects teeth and jaws that are positioned improperly. Teeth that are crooked or not in the right place can be less esthetic and might affects one’s smile and confidence .It also cause difficult to clean all the surfaces causing gum infection and dental caries .
What are the treatment option for this condition ?
HEALTHIER MOUTH
PLEASING APPEARANCE
BETTER BITING EFFICIENCY
Types of irregularity:

CROSS BITE

PROCLINED TEETH

SPACING

CROWDING
WAYS TO CORRECT TOOTH IRREGULARITY
CONVENTIONAL BRACES
INVISIBLE BRACES
CONVENTIONAL BRACES
Dental braces are devices used in orthodontics that align and straighten teeth and help position them into right place .commonly used is metal braces .if you prefer more esthetic options ceramic braces (tooth colour braces )can be opted which has similar efficiency as metal one.

HOW MUCH TIME DOES IT TAKE TO FINISH THE BRACES TREATMENT?
Time duration depends on the amount of problem or irregularity or need for tooth extraction .Generally orthodontic treatment takes around 10 months to 24 months .once a month visit will be required to direct the teeth in right position.
ALL THE ORTHODONTIC TREATMENT REQUIRES TOOTH REMOVAL?
Need for tooth removal (extraction) depends on the amount of jaw problem and how forwardly teeth is placed and how crooked the teeth are arranged. Orthodontist will evaluate the need for extraction only if teeth cannot be aligned without tooth removal.

BEFORE

AFTER


CAN ONE EAT NORMAL FOOD WEARING DENTAL BRACES?
Yes, one can have normal food during orthodontic treatment with slight modification to ones eating habit.Brackets are metal clips attached to teeth, which along with wire causes tooth movement .if brackets are broken desired tooth movement will not happen. Hence it is mantodatory to avoid very hard food like like nuts ,bones and sticky items like bubble gum. it better to cut the hard foods into small piece and eat .there is no restriction food like rice and upma or idly etc ..and no restriction for hot and cold food.
WHAT IS INVISIBLE BRACES?
Invisible braces (clear aligners ) are braces that suited for patient who very conscious about their appearance and do not want wires to be seen from their teeth all the time (e.g. people in media or teenage or adults who finds it awkward to show braces in the public). it one of the recent and break thorough in braces technology. where there is absolutely no wire or bracket present in the mouth .instead a clear plastic self removal tray set is given to patient to bring about tooth movement which they have to change themselves at home every month as per instructions of orthodontist .This is completely invisible and do not pose any social esthetic problem and oral hygiene maintenance becomes very easy and less dental visit.

AGE LIMIT FOR BRACES TREATMENT
There is no age limit for orthodontics .Even children from age 10 to late adult can go for alignment provided they have healthy teeth and gums
For children ,
Kids with irregular teeth alignment might affects normal growth of the jaw and affects esthetic appearance causing teasing by their friends or it can reduces kids confidence .hence orthodontic treatment might help them to regain better smile and cope with peer group.
Orthodontics treatment treatment can be intervened at early age as 10 years.

BEFORE

AFTER


Can Improper jaw /bite can be corrected early age ?
Generally ,Our mouth is made up who jaws upper (maxilla )and lower jaw .correct position of the both jaw in 3dimension will give pleasing look .if either of jaw is not positioned correctly might affects teeth and face giving the compromised smile.
If your kid has jaw problem or teeth alignment that affect the normal growth of the jaw,it is mandatory to start functional theraphy (type of dental treatment ) to allow or stimulate the normal growth which is around 9-11 years where kids growth is at maximum.if left untreated he/she might require surgery to correct jaw and bite at later stage.
There are lot of functional appliance ,based on the jaw problem and maturity of kid appliance is carefully selected.
Types of functional appliance


Can adults improve their bite or correct their forwardly placed jaw
SIGNS OF JAW PROBLEM
REDUCED UPPER INCISOR SHOW ON SMILING
MORE LOWER INCISOR SHOW PRESENT ON SMILING
FORWARDLY PLACED LOWER JAW OR TEETH
FLAT UPPER CHEECK
JAW SHIFTED TO ONE SIDE
CROSS BITE CAUSING DIFFICULTY TO EAT
Case 1 :

BEFORE




AFTER



Case 2 :

BEFORE




AFTER