Specialization
- Brachial Plexus
- Breast Surgery & Reconstruction
- Burns
- Burns
- Cancer Reconstruction
- Cleft Lip and palate
- Congenital Hand Differences
- Cosmetic Surgery
- Diabetic Foot & Chronic Wounds
- Hand and Wrist Surgery
- Lower Limb Reconstruction
- Lymphedema
- Maxillofacial Surgery
- Microsurgery & Replantation
- Microsurgery Lab
- Skin Bank
- Spastic Hand
- Super Speciality Courses & Fellowships
Brachial Plexus
A Special Clinic for the Management of Birth Brachial Plexus Palsy at Ganga Hospital
Ganga Hospital offers the services of a team of Hand and Microsurgeons, Anaesthesiologists and Physiotherapists having special experience in treating children with Birth Brachial Plexus Palsy (commonly also referred as Erb’s Palsy) for the last 25 years. BBPP or Erb’s Palsy as is commonly called, refers to weakness of the hand seen in children immediately after birth. No doubt it causes a lot of concern amongst the parents, since it is an unexpected event. It occurs once in 1per 1000 live births. This percentage remains almost the same even in developed nations and has remained so for decades showing that it has no relations to the quality of Obstetric care available in the society.
Advances in Hand Surgery and the advent of microsurgery offer so much to these children to make them better. The Department of Plastic, Hand and Microsurgery at Ganga Hospital is one of the leading centres in the South Asian region in this field in terms of volume, quality of work and team work in this field.
The Team Leads
Dr S Raja Sabapathy, MS., M Ch, FRCS Ed, DNB, Hon FRCS (Glasgow)FAMS, D SC (Hon)
Dr Hari Venkatramani, MS., M Ch. (Plastic), DNB (Plastic), EDHS (Euro. Board)
Dr Praveen Bhardwaj, MS (Ortho); DNB (Ortho); FNB (Hand & Reconstructive Microsurgery)
Mr Gopinath MPT, Chief Physiotherapist
The children with Brachial Plexus injury have varied needs. It may be from physiotherapy, to complex microneural and microvascular procedures to bone work. The team at Ganga Hospital has the capability to do the full spectrum

Fig. 1- A child with brachial plexus injury requires a team of experts for his/her optimal management and life changing recovery
Brachial Plexus is like a network of cables carrying electrical signals from brain to hand. Through this brain controls the function of the hand.
Many times birth canal may be narrow for a baby being born. In such cases there can be excessive stretch on neck during delivery which in turn stretches cables of brachial plexus causing injury.
Usually this will lead to paralysis of the hand. This can be temporary or permanent. It can be total or partial with fingers working but inability of baby to bend elbow and lift shoulder
Stretching of brachial plexus can injure it in a number of ways. Rupture means the nerve cable is cut after it has come out from main trunk from brain that’s spinal cord. Whereas avulsion means nerve cables have been pulled out of main trunk, spinal cord. The implication is that in case of rupture, the injured nerve can be joined back but when there is avulsion the injured nerve itself can not be joined, however the function can be still restored by recruiting some working adjacent nerve to the injured nerve.
Bones of babies are growing at a rapid rate. Normally, growing bones and joints have even pull due to different muscles from all sides but in case of brachial plexus as some muscles are paralyzed there is an uneven pull on growing bones and joints leading to deformities.
First thing is don’t panic. Majority of babies born with brachial plexus injury recover naturally. Once you are recovered from delivery and travel comfortably get baby seen by doctors treating these injuries, (hand or plastic surgeon). It is good enough to see the doctor even by about 6 weeks. The doctor would examine the child and record the recovery and will explain you the physiotherapy and the pattern of recovery expected which may differ from child to child.
Depending on how the baby is progressing surgery can be planned between 3 to 6 months but not all babies need surgery at that time.
Treatment depends on age of baby. Till 3 to 5 months it is better to wait and see if natural recovery occurs. If not then it’s time to think about surgery. During surgery the surgeons will look at the nerves to find the level of injury and assess the way to rejoin the nerve.
Botox is a medicine made from a bacteria, it causes temporary weakness of muscles. It has been commonly used in cases of spasticity and in cosmetic surgery and it also useful for some select cases of birth brachial plexus injuries as well. In babies with partial recovery from injury there can be imbalance between muscles and it may cause some deformities or may restrict some movements. Botox can be used to correct this imbalance and improve the movements. In some children the effects could be ever-lasting while other may need surgery to improve the function in future.
Yes, usually baby is admitted for Botox injection but more as a precautionary measure. Usually baby can go home in 1 day.
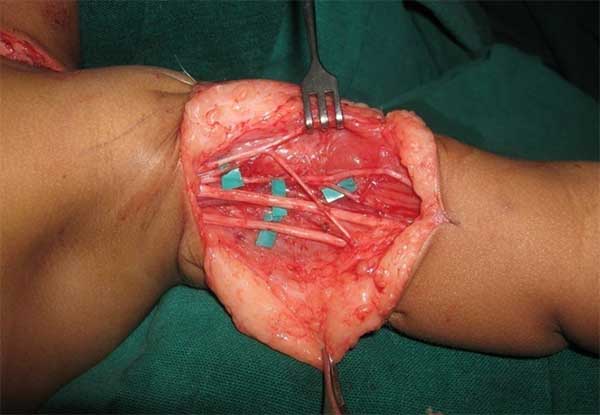
If at 3 to 6 months baby does not recover as much as doctors want, then there is a good chance that brachial plexus nerve cables are cut and need to be repaired. That is why doctors do an operation to actually see those nerves and if found cut repair them. Usually the damaged nerves will have a gap between the two cut ends and surgeon may take a nerve from the leg to bridge the gap. The leg will have no functional consequences as this is a dispensable nerve and children can normally run and play like any other child. Sometimes cables may be irreparable in which case doctors set up cross connections with nearby working nerves to get movement in shoulder and elbow. This operation is called nerve transfer.
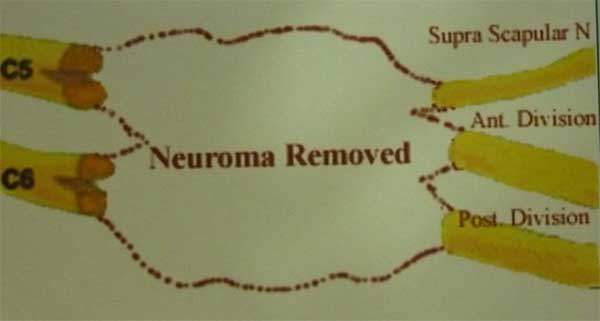
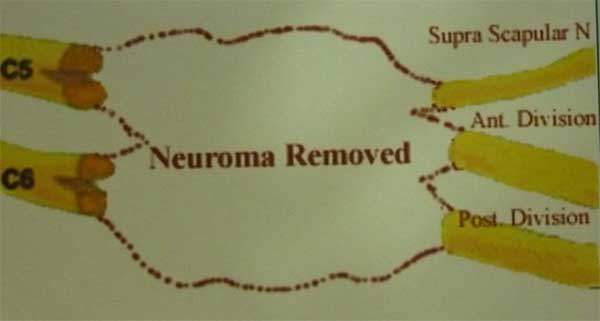
Fig. 2- Nerve grafting: The procedure involves removal of the injured nerve segments and reconstructing the gap with sural nerve grafts/ cables taken from the leg


Fig. 3- A child who underwent nerve grafting at age of 8 months. He achieved excellent improvement of the shoulder and elbow function and was able to enjoy normal childhood.


.jpg)
Fig. 4- Good improvement in the shoulder and elbow function in a child who underwent nerve surgery at age of 14 months (Pre-op above and Post-op below). He underwent nerve transfer surgery (Spinal accessory to suprascapular nerve, ulnar nerve fascicle to biceps and median nerve fascicle to brachialis motor branch transfer)
Free functioning muscle transfer is a surgery where doctors take one muscle from one area of body and put it in a new place where it will work to give some movement. The problem in brachial plexus injury is paralysis of muscles and if original muscles cannot be made to work again for reason of delayed presentation free functioning muscle is transferred to replace the paralyzed muscle.
Inability to lift arm can be due to paralysis of lifting muscles, too strong opposite pull from neighboring muscles or mostly a combination of the two. If paralysis is problem then exploration of nerves as described above can be done. But if neighboring muscles tightness is the problem then releasing this too strong opposite action by Botox injection or a surgery is required.
Mod Quad is a kind of soft tissue rebalancing operation designed to improve the shoulder movements. It improves lifting of arm in children who are unable to do so due to tight muscles in armpit. The tight and overly contracting muscles in the axilla (armpit) are relaxed and pressure on a nerve cable is released. Muscles are also transferred to restore balance as per the need of the child. Usually after this operation arm can be made to go over head and the children are able to perform the overhead activities much easily. Day to day activities like combing hair and selfcare become as simple as it should be.

Pre op

Post op
Fig. 5- A child who underwent Mod Quad operation. The pre-op and post-op images above show marked improvement in the range of shoulder movements

Pre op

Post op

Pre op

Post op
Fig. 6- Results of Mod Quad procedure
- 3 to 5 days.
After Mod Quad operation what do we need to do and when do we expect recovery? Ans: There will be a splint keeping arm up which needs to be kept in proper fitting for 2 -3 weeks. It is reasonably easy to take care of splint and doctors will demonstrate how to maintain it in position. After 3 weeks physiotherapist will show certain exercises to be done at home. Recovery takes up to 3-4 months.
Again treatment is dependent on child’s age. For children up to 6-7 years of age. Tendon transfer and Triangle Tilt Operation’ is helpful but for older children ‘Derotation Osteotomy of Humerus (arm bone)’ is required.
This operation is done to improve active outside rotation of the arm at shoulder. A functioning but expandable muscle is transferred to augment the function of weak external rotator muscle. This operation is possible if the joint is free of any tightness in young children.
3- 4 days. Plaster for- 4-6 weeks followed by physiotherapy. Recovery can be seen by about 3 months and it keeps getting better till one year. Children can start using the hand freely at 3 months after surgery.
Triangle tilt operation is designed to help shoulder to move in more normal way in cases where shoulder position and orientation is changed due to brachial plexus injury. In this operation shoulder joint is re-oriented to its normal position which allows the arm to rotate out and prevent future shoulder deformity. It is effective in very select group of patients and the doctor will examine the child and decide if this operation is needed.

Pre op

Pre op

Post op

Post op
3 to 5 days.
There will be a splint to support shoulder in its new position. Doctors will demonstrate how to take care of splint. Splint has to be maintained till 4 weeks after which a series of exercises are started. Recovery is expected in 2 – 3 months.

A) Pre op

B) Pre op

C) Post op

D) Post op
Fig. 7- Children who had severe ‘trumpet sign’ while trying to reach the mouth (a and b) and gross limitation of external rotation at the shoulder achieved good correction after the surgery.(c and d)
Derotation osteotomy operation is done to treat children older than 6-7 years having problem to rotate arm outside and having unnecessary lifting of shoulder when trying to get hand to mouth. In this operation arm bone is modified in a way that allows arm to rotate arm away from body.
4-5 days.
Child will have a plaster to operated arm for 4 weeks. After that exercises of operated hand started. Child can use hand for light work at 1 month, full use of hand is allowed after 2 – 2.5 months.

Pre op

Post op
Fig. 8 - Good correction of the hand to mouth reach posture with the humerus osteotomy in this child. The child was very conscious while eating lunch at school because of the awkward position of the arm while she reaches mouth. Now she was happy eating and sharing!
Doctors like to find out whether joints are stiff or smooth. If joints are smooth and muscles in forearm are working doctors can adjust the muscles so as to make palm face down but many times this itself may not be adequate and the orientation of the bone needs to be changed to get desired movement (Fig. 9, 10).



Fig. 9- The aesthetic and functional changeover following corrective osteotomy in a child who was unable to turn her palm downwards


Fig. 10 - Showing the improvement in the appearance and the function after the forearm osteotomy in this child. The procedure tremendously improved the child’s confidence and outlook to enable her to enjoy her childhood and now she is grown to becomes part of medical team.
Approach to this will be similar to above mentioned plan. Only things will be done reverse of above.


Fig. 11 - A child who is able to eat comfortably after we restored up turning (supination) of the forearm by tendon transfer surgery. Another child who was so thrilled to have been able to take the offerings at the temple in the right hand finally!
Usually if within 2-3 months fingers are not bending then early nerve surgery is recommended. Since the fingers are for away from the area of nerve injury the recovery takes longer time and often is not perfect however depending on what muscle are working other hand muscle can be shifted to make fingers bend .but if sufficient muscles are not available free functioning muscle transfer may be done for finger provided shoulder and elbow are stable.
In short, a child with birth brachial plexus palsy at any age can he helped in various ways to improve the function and eventually made capable to ‘look normal’ and perform all the day to day activities and enjoy life of a normal child and grow up to achieve whatever he wants to. We would love to help them to live their dream!