Brachial plexus is an intricate network of nerves formed by the coalesce of C5-C8 cervical and T1 thoracic roots from the spinal cord. The nerves arising from this complex network subsequently provide the movements and sensation to the entire upper limb. Injuries to the brachial plexus can be very disabling as they cause paralysis of the movement of the upper limb and preclude effective use of the upper limb. These injuries are caused by high velocity trauma like road traffic accident or fall from height. In India, two wheelers accident are the commonest cause and 90% of our patients have been victim of fall from two wheelers. Consequently, young adults are commonly affected with this injury. These injuries are ‘life altering’ as they may result in substantial physical disability, psychological distress and socioeconomic hardship. However, with the recent advances in the treatment of these injuries most of these patients can be helped and made better to an extent that they can lead an active and productive life and still achieve their future goal they aspired to before the injury.
The signs and symptoms vary greatly depending on the severity and location of the injury. An electric shock like feeling radiating down the arm with temporary weakness is seen with the mild injuries. Complete lack of movement, loss of sensation, severe pain and permanent weakness point toward a more severe form of injury.
The extent of spontaneous recovery following a brachial plexus injury is variable and unpredictable. It requires frequent and thorough clinical examination over the first three months after injury to look for the signs of recovery. 90% to 100% of mild stretch injuries (pure neurapraxia) would recover within this period. During this period, the patient will be asked to follow a physiotherapy protocol to keep the joints supple, prevent stiffness and strengthen the working muscles. The patient might be asked to undergo radiological (X-rays of chest and cervical spine, MRI) and electrodiagnostic (NCV, EMG) investigations to look for associated injuries and to define the extent and level of the brachial plexus injury.
Surgery is treatment of choice in patients who have not shown any spontaneous recovery in first 6-10 weeks. If there is some spontaneous recovery, observation period could be extended but surgical intervention should not be overly delayed as the outcome of nerve surgery is inferior if surgery is done after 6 months from the time of injury. Ideally, a global brachial plexus palsy needs surgery at about 2 months and partial brachial plexus injury at about 3 months in absence of any spontaneous recovery. Patients with complete plexus avulsion injuries where the chances of spontaneous recovery are low, surgery can be done with exploration and reconstruction at an earlier period between four to six weeks.The goal of surgical management is to restore the lost motor function i.e. to regain movements. The specific aim of the surgery would differ with the extent of injury the patient has, nevertheless, any restoration of movement will greatly improve activities of daily living and thereby quality of life. However, the surgeon and the patient must understand that the limb function may not return to pre-injury levels following the surgery.
Nerve regeneration happens slowly (1mm/day) and results following surgery takes a long time to be seen clinically. Surgeries performed beyond six months are associated with less favorable outcomes as the motor endplates of the target muscles start degenerating following denervation.
More than half of these patients with brachial plexus injury experience disturbing neuropathic pain. Nerve surgery often does not directly address the pain as the cause is at the spinal cord and brain level, but studies have shown that there is some reduction of pain following exploration of brachial plexus and neurolysis. It can be reduced to some extent with pharmacological measures (antidepressants amitryptaline, anticonvulsants- gabapentin, pregabalin) and intractable pain not responding to the pharmacological measures may need surgical procedures as last resort (dorsal root entry zone ablation) for some relief.
The surgical procedures can be any of the following depending on the type and severity of the injury:
Freeing up the nerve from scar tissue
The damaged part of the nerve is excised till the healthy nerve level and the gap in the injured nerve is bridged with nerves taken from other parts of the body (usually Sural nerve from the leg) providing a bridge for the new nerve growth over time.
In root avulsion injuries, the proximal cut end of the nerve is not available for repair. Hence, a part or whole of a functional, less important nerve (the donor) is transferred or connected to the non- functional more important injured nerve without any morbidity. The commonly used donors are spinal accessory nerve, intercostal nerves, phrenic nerves, contralateral C7, a part of normally functioning median or ulnar nerve.
In delayed presentation, partial/failed recovery of previous nerve surgery, a nearby functioning muscle can be used to restore the lost function by Tendon transfer operation. However, if no local muscle is available then a muscle from the thigh (gracilis) can be transferred to restore the function. This free functioning muscle transfer (FFMT) involves transferring a healthy muscle with its blood and nerve supply to the site of paralysis and is an effective operation in complex cases.
Permanent fusion of the joints (shoulder, wrist) in the scenario where no donor is available to restore the desired movement is an effective alternative.
Common patterns of presentation
In these group of patients, there will be weakness of shoulder abduction and external rotation due to paralysis of suprascapular nerve (innervating supraspinatus, infraspinatus muscle) axillary nerve (innervating deltoid and teres minor muscles). Such patients need surgical intervention if there is no recovery in about 3-4 months. This paralysis can be very effectively corrected by dual nerve transfer surgery, wherein, a motor branch of radial nerve to long/medial head of triceps is transferred to the axillary nerve and spinal accessory nerve is transferred to the supra scapular nerve


In these patients, in addition to the shoulder paralysis seen in C5 injury detailed above, there is loss of elbow flexion and supination because of paralysis of biceps and brachialis muscles. Elbow extension, wrist and hand function remain good in these patients. Such patients need surgical intervention if there is no recovery in about 3 months. Common operation done is such cases in the dual nerve transfer for shoulder as described above and dual nerve transfer for elbow flexion. The later involves transferring a small part of the normally functioning ulnar and median nerves (one fascicle) to the motor branches to the biceps and brachialis muscles respectively. The great advantage of this relatively newer technique over the conventional nerve repair operations is that the recovery is seen faster as the nerve repair is done very close to the target muscle. We expect to see improvement after this operation in about 4-6 months (Fig. 2a&b). The operation is effective in about 90% of the patients.


Along with the deficits mentioned in the above category, these patients exhibit lack of elbow extension, wrist extension and weakness of finger movements to variable degrees. These patients are treated with the same protocol and the nerve transfers include spinal accessory nerve to suprascapular nerve and Oberlin’s transfer after intraoperative confirmation of electrical activity in the donor nerves. In selected cases, ulnar nerve fascicle can be used to motorize the triceps. All these patients require secondary procedures for wrist and finger extension with tendon transfers or arthrodesis.



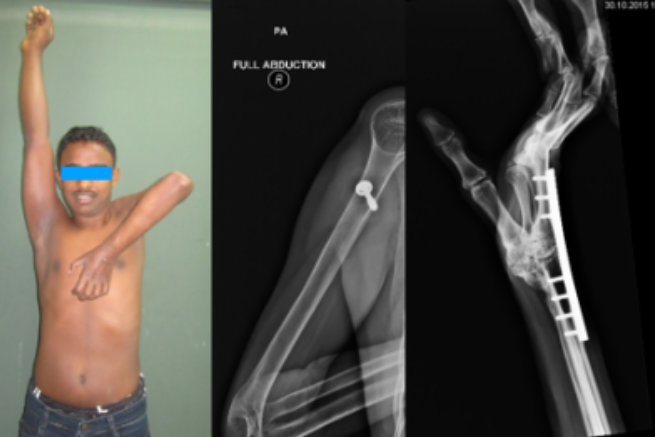
Restoration of elbow flexion in a patient with C5,6,7 palsy. Note the wrist and finger extension after tendon transfers
These patients exhibit a completely flail extremity, where the reconstructive options are grossly limited. They require staged reconstructive procedures. The first priority is elbow flexion, followed by shoulder stability and then the hand function. Elbow flexion is restored with nerve transfer surergy (spinal accessory nerve to musculocutaneous nerve) when the patient presents before 9 months from injury and if later, a free functioning gracilis muscle transfer has to be considered. Once the patient recovers elbow flexion power of grade 3 and above (MRC scale), he/she becomes eligible for the subsequent procedures namely, trapezius transfer/ arthrodesis of shoulder for shoulder stability and wrist arthrodesis. Finger flexion can be restored with free functioning muscle transfer or transfer of the recovered biceps (grade 4 and above) to the finger flexors.

Spinal accessory nerve to musculocutaneous nerve transfer- Pre-op and Post-op after 1 year
Post- operative management: Patients who underwent nerve surgery are advised for total immobilisation of the extremity for four weeks following which joint mobility exercises and electrical stimulation are started. They are provided printouts about the therapy and charting of the electrical stimulation to done twice a day. Patients who undergo trapezius transfer are immobilised in a shoulder abduction splint for two months and the started-on physiotherapy thereafter. Patients undergoing tendon transfers are asked to review the hospital for supervised physiotherapy sessions at one-month post-surgery.
Results of trapezius transfer and wrist arthrodesis

Free functioning muscle transfer for finger flexion with results after 1 year
In summary, brachial plexus injuries are complex with variable extent, severity and presentation. They need detailed assessment and planning by the experienced team. The surgical options needed for a given patient also vary immensely needing expertise in Orthopedics, plastic surgery and Microsurgery. Brachial plexus Surgery team at Ganga hospital provides a comprehensive ‘complete’ solution to all the brachial plexus related problems. With experience of managing more than 2000 patients with brachial plexus injury this team is world renown in this field of Hand and Reconstructive Microsurgery. Brachial plexus injuries are surely ‘life changing’ injuries but surely with the growing expertise in this field for almost all the patients with this injury there is hope!