Specialization
- Brachial Plexus
- Breast Surgery & Reconstruction
- Burns
- Burns
- Cancer Reconstruction
- Cleft Lip and palate
- Congenital Hand Differences
- Cosmetic Surgery
- Diabetic Foot & Chronic Wounds
- Hand and Wrist Surgery
- Lower Limb Reconstruction
- Lymphedema
- Maxillofacial Surgery
- Microsurgery & Replantation
- Microsurgery Lab
- Skin Bank
- Spastic Hand
- Super Speciality Courses & Fellowships
Hand and Wrist Surgery
The human hand is one of the marvels of evolution, unsurpassed in its dexterity and sophistication. Naturally special skills and knowledge are needed to put it back to work when a problem happens to the hand, be it an injury in the workplace or an infection. When children are born with hand deformities, it calls for ingenuity to make it functional.
Till recently, hand problems were managed by all surgeons. With the advent of microsurgery and enhanced knowledge of the mechanics of hand function, Hand Surgery as a speciality began to evolve. Plastic surgeons and Orthopaedic Surgeons were attracted to this field. Better results are now obtained when surgeons who are trained in Hand surgery deal with the problems of the hand.
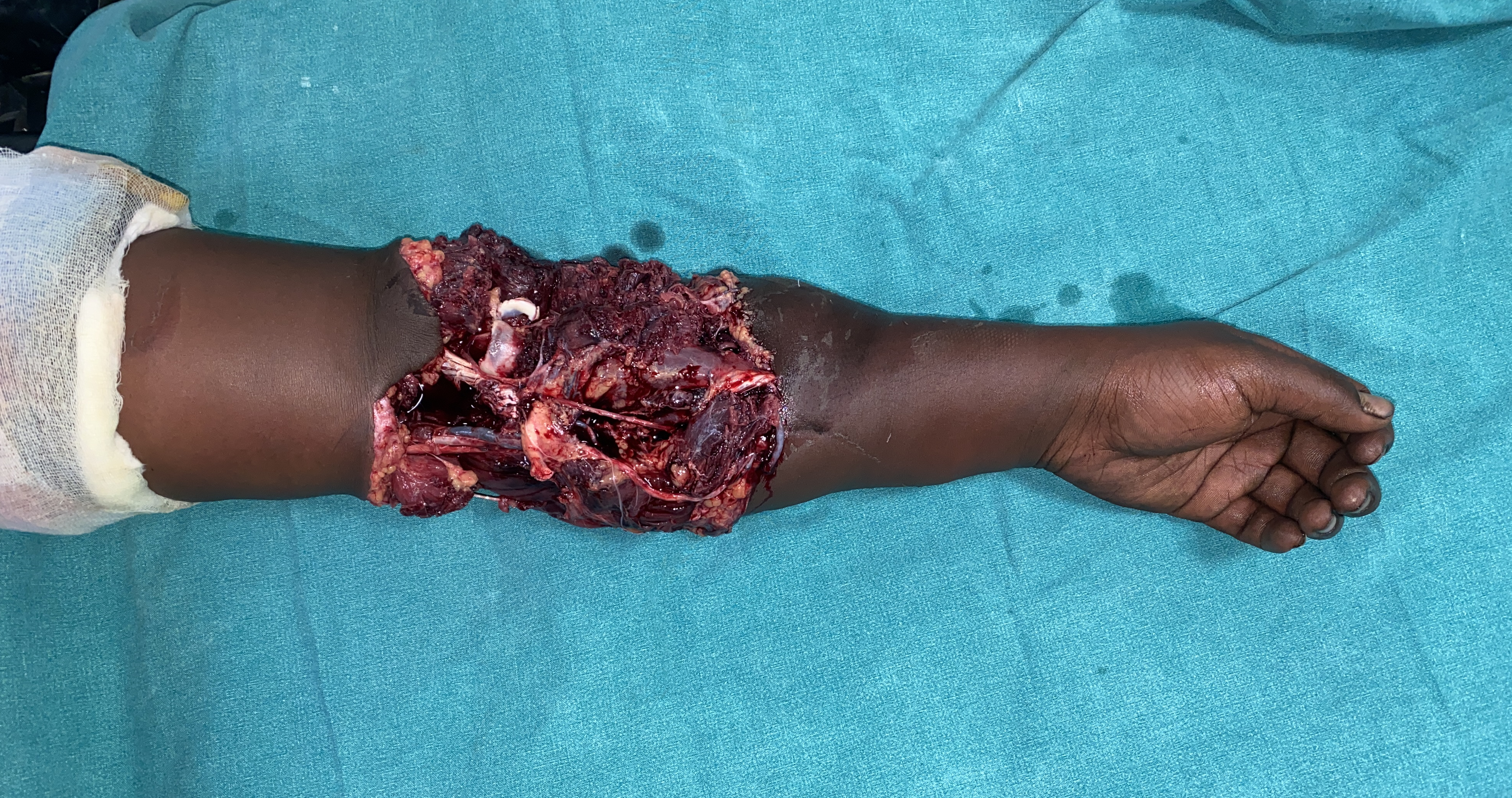
Why do raw areas over the upper limb occur?
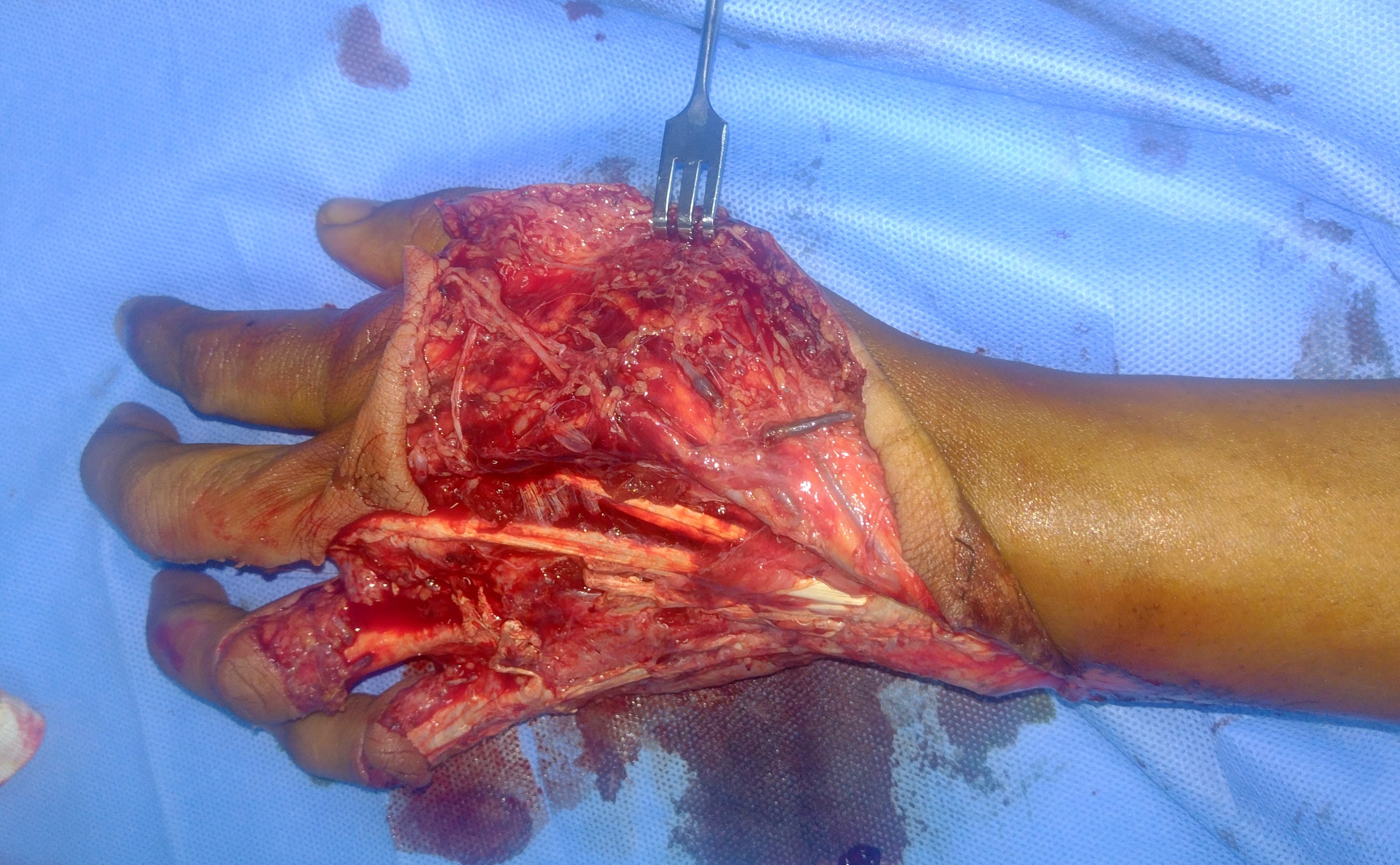
Raw areas over the upper limb predominantly occur due to trauma, infection and burns. These raw areas need to be treated well and at the right time to avoid infection, for the wounds to heal well and for the hand to function well.
How soon and why should raw areas over the upper limb be treated?
Raw areas over the upper limb should be treated as early as possible. The raw areas should be cleaned early (debridement) on seeing the patient and should ideally be closed within 72 hours from the debridement procedure. Covering the raw areas early would decrease the pain, swelling, stiffness of the fingers, infection, thick scars and eventually give useful function of the hand and upper limb.
What do you mean by debridement, and why is it important?
Debridement is the removal of all dead and non-viable material from the wound such as dirt, mud, dead tissues, pus and other infected tissues. This is one of the most important steps in the reconstruction of the limb because reconstruction and covering raw areas can only be done when the bed is clean, does not contain dead tissue and has only healthy tissues with good blood supply at the base. Debridement is done best by a surgeon with good magnification, proper anaesthesia and good light. At Ganga Hospital, we debride the wounds under good magnification with surgical loupes, excellent anaesthesia by a round the clock anaesthesia team and good lighting at any given time and day of the year. As we operate daily, we close the wounds within 72 hours from debridement to give good results.
What do you mean by “Graft”?
A graft is a piece of tissue which does not have its own blood supply and depends on the bed for its blood supply.
What do you mean by “Flap”?
A flap is a piece of tissue which has its own blood supply and does not depend on the bed for its blood supply. When fractured bones, dried bone, tendons or plates and screws are exposed, they do not have any blood supply, and hence a flap which has its own blood supply needs to be done to cover these structures.
Graft
What is a skin graft, and how is it done?
The skin consists of the outer epidermis and inner dermis. A skin graft consists of the outer epidermis and a part of the dermis. Under anaesthesia, skin grafts are taken by a device known as the Humby’s knife or dermatome. The skin graft taken is then placed on the recipient site and anchored over the raw areas using either sutures or skin staples. The skin graft needs to be in close contact with the bed, and snuggly fitting dressings are done to keep the graft and the recipient in close immobile contact. In the donor area from where the skin is taken, dressings are done. The remaining skin appendages of the donor skin after skin graft harvest tends to re-epithelialise and heals by itself within two weeks.



How does the skin graft heal and how long does it take to heal
In the first 2 days, nutrients diffuse from the recipient bed into the graft. In the next 2 days, vascular connections are established between the graft and the host vessels and from the fifth day, there is a good equilibrium of blood flow from the graft and the host vessel. It takes almost 3 weeks for the graft to settle well.
How long does the surgery take?
The duration of surgery depends upon the size of the wound, the time needed for wound preparation before grafting and method of graft fixation. For small and moderate size wound, the surgery takes about 1 to 1½ hours (excluding anaesthesia time). In case of extensive raw areas needing grafting like burns, and raw areas involving multiple areas of the body it may take around 2 to 3 hours. Each case may vary and may need discussion with the treating doctor.
How long do we need to stay in the hospital?
For the graft to take well, the graft must be in close immobile contact with the bed. We would not like to disturb the graft much. Hence we would like to discharge the patient around 5 to 7 days. By this time we will usually change the dressing twice.
What do we need to do to take care of the graft after it takes?
The limbs can be mildly swollen after application of skin grafts, and hence it is advisable to wear compression garments for a few weeks. Both the skin grafted area and the donor area are very dry, and hence moisturising creams or coconut oil is applied to avoid itching and skin excoriation. It is preferable to avoid sunlight over the grafted area to avoid hyperpigmentation. This is so especially when the skin grafted area is over the face.
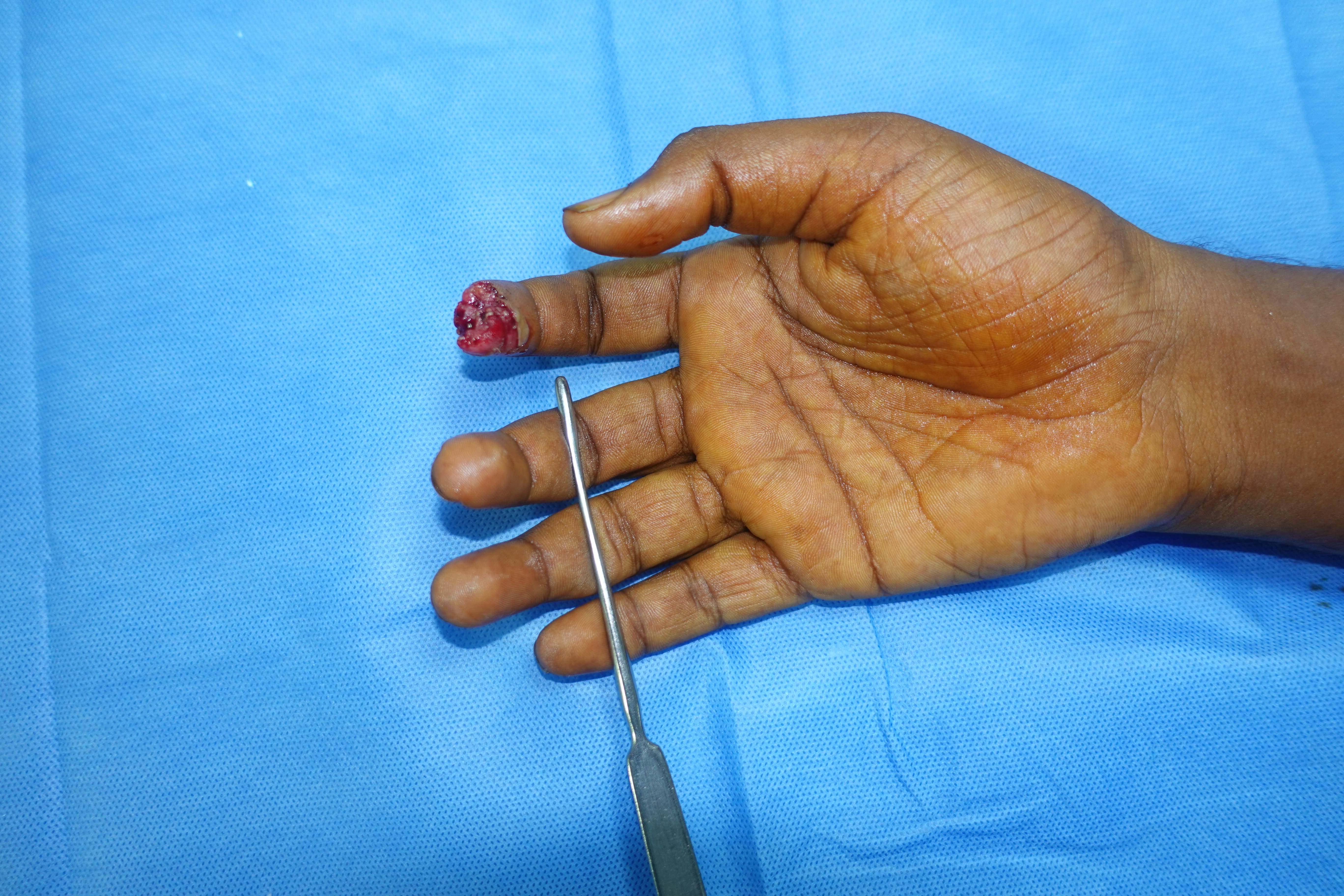
Flap cover over fingers
Straight VY Flap cover



How is this surgery done?
A “V” shaped flap is marked over the pulp of the fingertip, and this flap is advanced to cover the exposed bone. The donor area is then closed in the form of “Y” shape.
When do we do Straight V Y flap?
In fingertip injuries, Straight VY flap is done to cover the exposed bone when the palmar skin is longer than the dorsal skin. By performing the Straight VY flap, we can maintain the length of the finger, which would have become short if we performed a shortening and closure of the finger.
How long does it take to do the operation?
The operation takes about 30- 45 minutes
When do we come to remove the sutures?
The sutures can be removed in 10 to 14 days from the date of the operation.
Will there be sensations at the tip of the fingers after the operation?
Yes. There can be altered sensations at the tip of the fingers initially. The flap will regain sensations with time, and it will get better.
When can the patient go back to work?
The patient can go back to work three to four weeks from the date of operation.
Oblique Triangular flap

How is this surgery done?
An oblique triangle shaped flap is elevated from the palmar aspect of the finger based on the digital artery and nerve. This flap is then advanced to cover the wound and exposed bone. The donor area is then closed in the form of “Y” shape.
When do we do Oblique Triangular flap?
In fingertip injuries, Oblique Triangular flap is done to cover the exposed bone when the fingertip cut is oblique. By performing the Oblique triangular flap, we can maintain the length of the finger, which would have become short if we performed a shortening and closure of the finger
How long does it take to do the operation?
The operation takes about 45 minutes to 1 hour
When do we come to remove the sutures?
The sutures are removed about 10 to 14 days from the date of surgery
Will there be sensations at the tip of the fingers after the operation?
Yes. There can be altered sensations at the tip of the fingers initially. The flap will regain sensations with time, and it will get better
Cross Finger flap




How is this surgery done?
The desired flap is marked on the back surface of the adjacent finger (mostly in and around the middle segment). Then the flap is elevated and turned over like a page of a book and is sutured to wound over the injured finger, thus keeping the two fingers attached to each other. The donor wound is covered with a skin graft
When do we do Cross finger flap?
In fingertip injuries, Cross finger flap is done to cover the exposed bone when the dorsal skin is longer than the palmar skin. By performing the cross finger flap, we can maintain the length of the finger, which would have become short if we performed a shortening and closure of the finger
How long does it take to do the operation?
The operation takes about 1 hour
Do patients find it very uncomfortable to have both fingers fastened with each other?
After the initial operation, the hand is kept in a slab, and the patients feel very comfortable after the operation.
When do we come to divide the flap?
In two weeks from the initial surgery, the flap bridge is separated by another operation and fingers are separated
Will there be sensations at the tip of the fingers after the operation?
Sensations might not be present immediately after the operation. However, the sensations will slowly regain and will improve with time.
Commonly used flaps over the Upper limb
Posterior interosseous artery flap



How is this surgery done?



How is this surgery done?
The flap is marked over the dorsum of the mid-third forearm. It is then elevated along with the posterior interosseous artery, rotated to cover the raw areas over the dorsum of the hand or in the space between the thumb and the index finger. If the elevated flap is a small flap, it is primarily closed. If the donor area is large, the defect is closed with a graft.
When do we do Posterior interosseous artery flap?
Posterior Interosseous artery flap is done to cover small to medium-sized wounds over the dorsum of the hand and to provide extra tissue in the space between the thumb and the index finger.
How long does it take to do the operation?
The operation takes about 2 ½ hours
When will the flap settle?
The flap heals in about 2 weeks. Sutures are removed, and compression garments and physiotherapy is started to reduce oedema
How long do we need to stay in the hospital?
The hospital stay for the flap is about one week. However, the time needed to stay in the hospital can also depend on the underlying problem that the patient has.
Abdominal flaps/ Groin Flaps


How is this surgery done?
The pattern of the raw area of the flap is marked on the abdomen. The hand is brought closer to the abdomen, and in a comfortable position, the abdominal flap is raised and is stitched to the abdomen. The donor area over the abdomen is either primarily closed or is covered with a skin graft.
When do we do Abdominal flaps?
Abdominal flaps are done to cover small to large raw areas over the hand and upper limb. The advantage of doing abdominal flaps is that it facilitates easier subsequent operations in the upper limb. If we need to do a free flap later for bony support or for an extra muscle to move the fingers, the abdominal flap done earlier does not sacrifice any blood vessel and hence makes it easier to do the subsequent free flap.
How long does it take to do the operation?
The operation takes about 2 ½ hours ( excluding anaesthesia time)
As the hand is attached to the abdomen, will it be very uncomfortable or painful?
All our patients including children tolerate this procedure very well. While performing the abdominal flap, we plan in such a way that the hand is kept in a comfortable position. The hand is initially strapped to the abdomen by plasters for 3 to 5 days by means of plasters. Later the plasters are also removed. Patients don’t pull the hand from the abdomen as it can be painful if they do so. We start shoulder and elbow physiotherapy the next day after operation. In 2 days after the operation we try to make the patient stand, and we tend to mobilise the patient on the third day.
When will the flap be divided?
The abdominal flap is divided three weeks after the operation. In some patients, before we divide the flap from the abdomen, we may divide the flap in 2 stages. In the first stage, only part of the flap is divided, and in the next stage, the entire flap is divided. This is done to increase the vascularity of the flap and to make it more robust.
After the division of the flap, when will the flap fully heal?
Two weeks after flap division, all sutures can be removed. The flap will take about 6 to 8 weeks for it to settle down completely. Patients may need compression garments or crepe bandage to reduce oedema in the upper limb.
Can physiotherapy be done while having the flap connecting the upper limb to the abdomen?
Physiotherapy of fingers is still possible when the flap is attached to the body. Physiotherapy is promptly initiated for shoulder and elbow the next day after operation.
If my flap is bulky when can the flap be de-bulked?
The flaps can be initially bulky as we are taking abdominal fat. However, after all other procedures in the upper limb are over, we can debulk the flap in one or two stages. Else we can also suck out the fat in the flap by liposuction.
How long do we need to stay in the hospital?
The hospital stay for the flap is about 1 week. However, the time needed to stay in the hospital can also depend on the underlying problem that the patient has.
Free flaps ( Anterolateral Thigh flap/ Gracilis free flap)
When do we do free flaps?
Free flaps are done to cover medium to large areas of the upper limb.
How is this surgery done?
Gracilis flap is done by harvesting a muscle from the opposite thigh along with the blood vessel that supplies the flap. The anterolateral thigh flap is done by harvesting skin, fat and partly a small muscle from the outer thigh along with the blood vessels that supply the flap. The blood vessels associated with these flaps are connected to the blood vessels in the upper limb by microsurgery and are used to cover the defects.
How long does it take to do the operation?
This procedure takes about 3 to 5 hours to complete the procedure.
How successful is the flap?
In our set up, we have a success rate of 97 to 98%.
What is done to cover the defect over the donor area?
In gracilis free flap, only muscle is taken, and hence the donor site is closed primarily. Most cases of anterolateral thigh flaps may require skin graft at the donor site.
How is the patient managed after the operation?
The patient is shifted to the micro post-operative ward where trained nurses monitor the flap every 2 hours to see whether the flap is doing well for the first 4 to 5 days after the operation. The patient is then shifted to the ward. Patients generally get discharged around 2 weeks from the operation.
What do you mean by “Enchondroma”?
Enchondroma is a non- cancerous tumour that arises from cartilage found inside the bones.
How do they present?
Enchondromas present most commonly as painless swellings in hand and foot. Occasionally they can pain if the size of the swelling is large or if there is a fracture of the enchondroma.
How are they diagnosed?
Most of the enchondromas are discovered with X-rays following the development of pain or pathological fracture.
Is Enchondroma a cancer?
No. Enchondroma is not cancer. The risk of malignant transformation is very less (Less than 1%)
If I leave this untreated what will happen?
The bone can fracture with trivial trauma producing pain (Pathological fracture) and can turn into cancer ( Less Than 1%)
How is this condition treated?
Symptomatic enchondromas are treated by curettage(scraping out the tumour). The resultant bony defect can be left empty or grafted with bone grafts from the patient’s hip to give more stability.
If the enchondroma produces a pathological fracture, how is it treated?
The fracture will be usually allowed to heal before treating the tumour. The tumour will then be curetted out to prevent another fracture.
By taking bone from the hip, will the patient have any difficulty in walking?
The patient might find difficulty in walking for initial 2-3 days due to pain at the surgical site which will gradually improve without any resultant deficit.
Will the patient have pain and if so, how long does the pain last?
Pain at the surgical site and bone graft site is expected to be present for 2-3 days after surgery which will be taken care of with painkillers.
How long will I need to be in plaster after the surgery?
Following curettage and bone grafting, the limb will be immobilised in a below-elbow plaster for a period of 4- 6 weeks.
How is the patient managed after operation?
The patient is expected to stay at the hospital for 2 to3 days following the surgery. The patient stays until he feels comfortable walking. Sutures will be removed at two weeks from surgery followed by regular visits once every two weeks until 6 weeks.
Facts at a glance
| Duration of Surgery | Type Of Anaesthesia | Days of Hospital Stay | Suture removal | Return to work |
|---|---|---|---|---|
| 2 - 3 hours | General / Regional anaesthesia | 2 - 3 days | 2 weeks | 6 weeks |
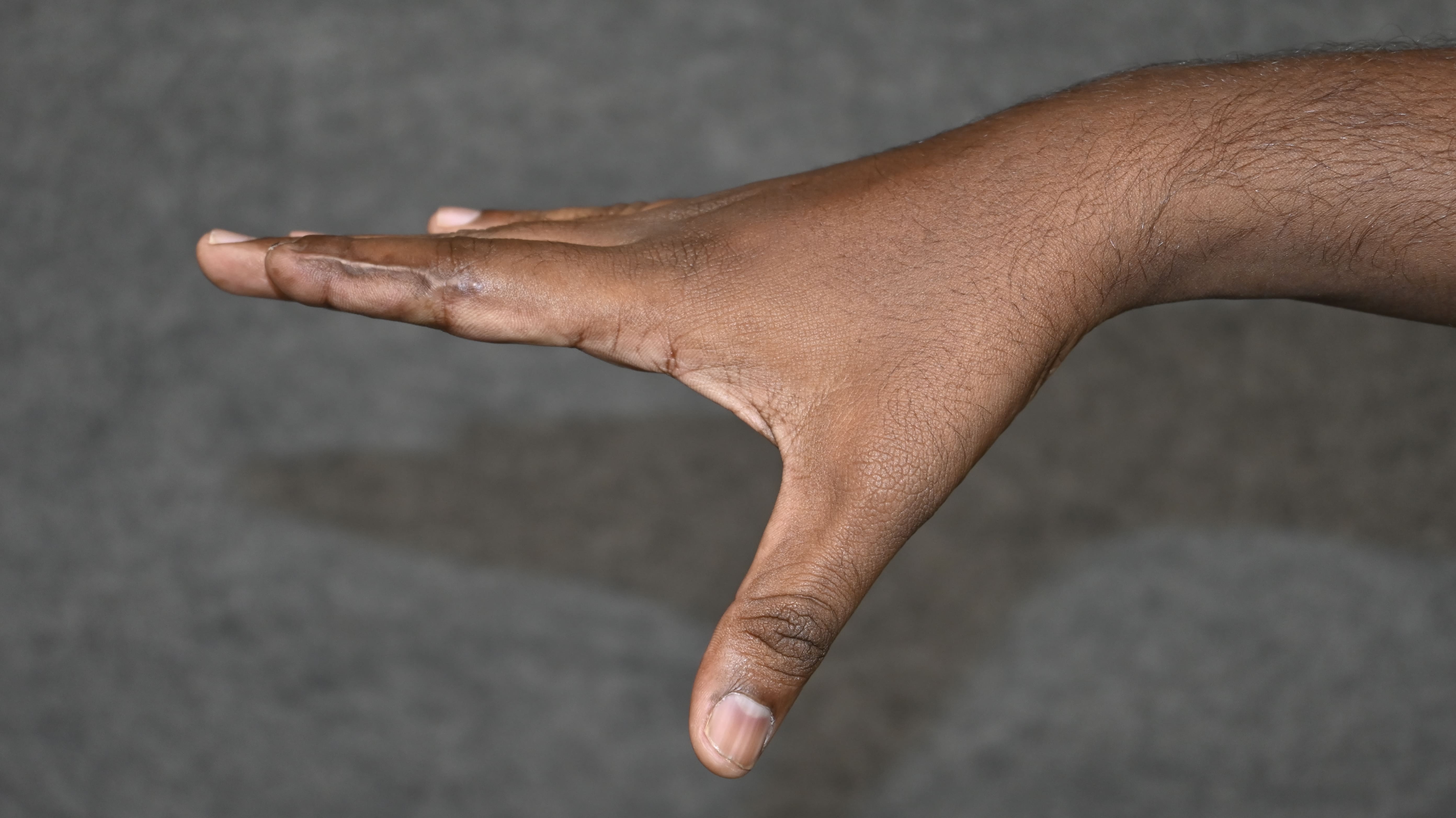
What is thumb hypoplasia?
Thumb hypoplasia is underdevelopment of the thumb. This underdevelopment can range from a smaller thumb to a totally absent thumb. In addition to a smaller thumb, it may present with weak ligaments, absent muscles, reduction of the space between the thumb and the index finger and some abnormalities of the forearm.
Why is the thumb important?
The hand functions well when the thumb meets the other fingers. The total absence of thumb results in about 40% loss of hand function. It is tough to pinch or grasp any object without a thumb. Hence it is essential to have a thumb which is stable, sensate and is in the right position.
Why does this happen?
The exact reason Is not known. It is postulated that this happens due to several factors like genetic, environmental and harmful medications taken during pregnancy
How common is this condition?
This condition is present in about 1 in 1 lakh babies. Boys and girls are equally affected. Both sides can be affected in 60% of cases.
How is this condition treated?
The treatment depends on the severity of the underdevelopment of the thumb. In mild cases with a smaller thumb, the parents are reassured that no treatment needs to be done. Patients who present with a narrow gap between the thumb and the index finger need a release of this space and cover with a flap. This would allow the child to hold bigger objects. If the muscles of the thumb are weak, strength could be provided by transferring a stronger tendon from nearby area. If the ligament in the base of the thumb is weak, it needs ligament reconstruction. However, if the joint at the base of the thumb is absent, attempts at local reconstruction have given poor results universally. Transfer of the index finger to make the thumb provided much superior results. This procedure is called Pollicisation. The same operation is also applicable for children with rudimentary floating thumbs and in the total absence of thumb.
If we are converting the index finger into the thumb (Pollicisation) will there be any difficulty in using the hand?
Children find it very comfortable in using the index finger as the new thumb. The hand functions better, and children feel more confident. The hand also looks better, and many people don’t notice one finger missing at a passing glance. How many of us have noticed that the famous Mickey mouse has only 4 digits?!!!
At what age can we do surgery?
At about 2 years of age
Do we necessarily need to undergo surgery?
It is better to undergo the surgery early as pollicisation not only enhances the function of the hand but also improves appearance of hand , thus boosting the confidence of the child.
How long do we need to stay in the hospital?
The child needs to stay in the hospital for approximately 5 days. The next dressing is done at 12-14 days from the surgery and a new plaster cast is given. The child is then seen between 2-3 weeks later. At 4-6 weeks from the operation the plaster cast is changed to a removable plastic splint and physiotherapy is started.
What will be the post-operative protocol for pollicisation?
After surgery, an above elbow plaster is applied with the elbow flexed for 2 weeks. This is done to prevent the child from disturbing the operated area and provide good hand elevation for better healing. Suture removal is done under sedation after 2 weeks, and a new above elbow case is applied. At 4-6 weeks post-surgery the plaster is changed to a removable plastic splint and physiotherapy is started. The child is advised to move the new thumb. When the child is not moving the thumb a short thumb splint is provided for further protection which is continued for another 4-6 weeks. Child will need physiotherapy and re- education for several months as there may be absence of representation of thumb in brain (in congenital absence). Later the child learns to use the new thumb without any difficulty
Tendon transfer
Following a tendon transfer a plaster cast is generally applied straightaway is much swelling is not anticipated after the surgery. This plaster is removed at 4-6 depending on the type of tendon transfer done and is changed to a removable splint and physiotherapy is started. It is good to do the initial training at our hospital as teaching a new movement to a child is challenging. Generally children take about 4-6 weeks to learn the new movement and incorporate in their normal hand use. All the supporting splints are off at about 3 months post surgery and the child can use the hand freely.
When will the wounds fully heal?
The wounds are expected to heal by 2 weeks from surgery however the plaster cast is generally needed for about 4-6 weeks.
Will the fingers grow after surgery?
Yes. The transferred index finger will grow as the child grows.
Facts at a glance for pollicisation (The facts could vary as per each case and needs to be confirmed with the doctor)
| Surgery time | Type Of Anaesthesia | Hospital Stay | Children Resuming playing | Suture removal |
|---|---|---|---|---|
| About 2-3 hours | General anaesthesia | 5 - 7 days | 3 months | At 2 weeks under anaesthesia |
Why does this happen?
During development, there are a number of signalling pathways which control the formation of the four fingers and thumb. When there is an error in these signalling pathways, an extra thumb is formed.
How common is this condition?
Thumb duplication can occur in 1 out of every 1000 live births.
If we plan to have another child, what are the chances that the other child will also have it?
There is a 50 percent chance of having an another child with this condition.
How can we treat this condition?
Thumb duplication can be treated by removing one digit of the duplicated thumb. One side of the tendons, ligaments and skin is preserved and the other side of the thumb consisting of bones, ligaments and soft tissues are reconstructed to make a well formed stable thumb.
At what age can the surgery be done?
We prefer to do the surgery when the child is beyond 1 year of age. There is no upper limit for surgery.
Which thumb will you retain and why?
The part of the thumb towards the index finger is usually preferred as it is generally bigger and the ligaments of the thumb towards the index finger is stronger. However, this may vary from patient to patient and is discussed with the patient before surgery.
Will there be any problems in moving the joints of the thumb after the operation?
After the operation, there might be some stiffness of the joints of the thumb. However the thumb will be stable and the patient will be able to do all activities.
Do we necessarily need to undergo surgery?
Not all duplicated thumbs neend surgery and many people are comfortable with a duplicated thumb. However surgery can give rise to a stable thumb which looks better and doesn’t get caught in various objects while using the hand.
How long do we need to stay in the hospital?
The patient would need hospital stay for 2 to 3 days..
What will be the post-operative protocol? (Need to mention that dressings will be done under sedation )
The operated limb will be protected in an above elbow cast which will be removed under sedation at 2 weeks. The reconstructed thumb will be protected by a splint for a period of 4- 6 weeks following which gradual mobilization will be started.
When will the wounds fully heal?
The wound are expected to heal by two to three weeks from surgery.
Will the thumb grow after surgery? Will the child be able to use the hand normally after that?
The thumb will grow after surgery. The child will be able to use thethumb to do all activities and will not have any restrictions for that.
Facts at a glance (The facts could vary as per each case and needs to be confirmed with the doctor)
| Surgery time | Type Of Anaesthesia | Hospital Stay | Children Resuming playing | Suture removal |
|---|---|---|---|---|
| 2 hours | General anaesthesia | 2 to 3 days | 8 - 12 weeks | 2 weeks |
What is Volkmann’s Ischaemic Contracture?
Volkmann Ischaemic Contracture is a deformity of the fingers, hand and wrist which occurs as a result of the shortening of the musculotendinous units of the upper limb due to inadequate blood supply.
Why does Volkmann’s Ischaemic Contracture happen?
Volkmann ischaemic contracture occurs in some closed fractures of the forearm, burns, snakebite or due to tight bandaging. In these situations, as the pressure in the forearm increases, the blood supply to the muscles reduces. This reduction in the blood supply can result in scarring and contracture of the musculotendinous units of the forearm. Hence the hand, wrist and fingers are kept in a flexed position. The nerves can also get damaged due to encasing and scarring of the musculotendinous units and reduced blood supply resulting in decreased or absent sensations in the hand.
How does Volkmann’s Ischaemic Contracture present?
Volkmann Ischaemic contracture presents with the following features
Flexed position of the fingers and wrist
Inability to straighten the fingers and wrist with compromise in the functioning of the hand
Decreased or absent sensation in the hands
Reduced or inadequate soft tissue cover in the forearm
History of injury a few months back
How can Volkmann’s Ischaemic Contracture be treated?
In mild cases, physiotherapy, stretching exercises and splints can be tried for three months. However most cases are severe and need a staged approach. In the first operation, the forearm is explored, and the scars in the musculotendinous units of the forearm which prevents extension of the fingers and wrist are excised so that the wrist and fingers are brought back into the right position. In the same operation, the nerves are also freed from the scars. If the surrounding soft tissue is inadequate, a flap is done so that subsequent operations can be done. The fingers and wrist are mobilised by physiotherapy. Once all the wounds heal, in a few months, another surgery is necessary to make the fingers flex. This is done by transferring an extra tendon needed to extend the wrist to the flexors of the fingers [ECRL to FDP transfer]. In severe cases where the extensor tendons are also involved, a muscle from the thigh (gracilis) is brought along with its blood supply and nerve supply and connected to the blood supply and nerves of the forearm to allow flexion of the fingers ( free functioning muscle transfer)
What is the interval between each surgery?
The subsequent surgery is done when the wounds of the previous surgery have healed well, scars become soft and supple, and physiotherapy has kept the joints of the fingers free. This takes about three months.
How important is physiotherapy?
Physiotherapy is essential to keep the joints supple, improve the range of motion of the joints and to strengthen the muscles which are working well so that they can be used for tendon transfer surgeries later. Ganga Hospital has a very good physiotherapy department who specialise in hand surgery. Frequent supervised sessions of physiotherapy are essential for the hand to function well.
When will sensations return back after surgery?
After the release of the nerves from the scar tissue, sensations can be expected to come within a few months. Return of sensations begins as altered sensations before good sensations are got. If the surgery is done early after the initial injury, the return of sensations is said to be better.
What is a “Toe Transfer Operation”?
The hand functions well when the thumb meets the other fingers. The toe represents the best substitute for a missing thumb or finger which may be lost due to trauma, burns or cancer. In case all five fingers are lost a toe can be transferred to the thumb and another toe can be transferred to the fingers.
How is a “Toe Transfer” Operation done?
Either the big toe or the second toe is harvested along with the tendons, blood vessels and nerves. The ball of the big toe needs to be retained, and hence the big toe is harvested only beyond the ball of the big toe. The second toe can be taken along with the bone more proximally. The gap between the first and the third toe is neatly closed so that normal appearance of the foot is maintained. In fact, once the scar settles well, at first glance many people don’t realise that a toe is missing once the wounds heal well. The harvested toe is anchored to the site of missing digit with K- wires. The tendons, blood vessels and nerves of the transferred toe is connected to the tendons, blood vessels and nerves of the hand to make it function like a new finger..
Is there any age limit for toe transfer?
Toe transfers can be done comfortably beyond 4 years of age in children. We tend to do it at this age as the structures can be very small earlier. Generally, there is no upper limit for the age of toe transfer as long as the patient is fit for surgery.
Which toe is taken for Toe Transfer and why?
When the length of the toe needed to be transferred is less, especially for the thumb, the big toe is preferred. When the length of the toe to be transferred is more or if a smaller size finger is desired, then the second toe is transferred for thumb reconstruction. The pros and cons of taking either the first or second toe is decided on case to case basis according to the hand and will be spoken to in detail during the consultation.
By taking a toe, will the donor foot look bad?
The big toe donor defect can be conspicuous but are acceptable. Second toe transfers carry negligible donor site issues and are mostly unrecognisable and are quite acceptable aesthetically.
Will the patient be able to wear regular shoes and chappals after the operation?
Following big toe transfer, the patient may not be able to wear slippers with a stem between the big toe and the second toe. Otherwise, they will be able to wear all kinds of slippers and shoes. Patients for whom second toe transfer is done have no problems in wearing any kind of footwear.
Will the child or adult be able to walk well after the operation?
Patients can walk well even without all the toes. Patients can walk, run and play after the operation also even if we take the toes. In fact, the popular cricketer Martin Guptill has only 2 toes in his left foot. So there is no disability without a single toe.
How many days after the operation will the patient be able to walk?
The patient can start walking without weight-bearing in 3 weeks. At 4 weeks full weight-bearing can be allowed.
Will Toe transfer operation be done in a single-stage or in multiple stages?
When the length of the finger to be replaced is less, we may be able to do the toe transfer operation in a single stage. However, if the length of the finger to be replaced is more, we may have to first give soft tissue cover for the thumb or the finger in the first stage in the form of an abdominal flap. Here the hand is kept attached to the groin through the abdominal flap, and it is divided in 2 stages in the 3rd week and 4th week. When the flap heals well we do the toe transfer operation which can take approximately 3 months from the initial operation.
After transferring the toe to the hand, will the toe be able to move and when can we expect this?
This operation aims to make the thumb meet the fingers so that the hand would be useful. The tendons of the toes are connected to the tendons of the hands to make it function. We start mobilising the transferred toe after 4 weeks. The patient would need regular supervised physiotherapy for them to achieve good results. We expect the transferred toe to move well in 8 to 12 weeks after the operation.
After transferring the toe to the hand, will the toe be able to feel and when can we expect this?
Recovery of sensations is usually good. In about 6 to 8 months, the patients tend to get some sensation, and it gets better with time.
How long will we need to stay in the hospital?
The patient would need to stay in the hospital for about 10 to 14 days after the procedure.
What is the post-operative protocol?
Since this is a microsurgical procedure involving the connection of minute blood vessels of size of about 1mm, we need to monitor the transferred toe. Hence we monitor the viability of the transferred toe in a special microsurgical post-operative room where the patient is kept warm, and there are trained nurses who keep checking on the viability of the flap. The first dressing is done under anaesthesia 2 weeks from the toe transfer surgery. The cast and the sutures are removed, and a slab is applied. We remove the K-wire in 4-6 weeks and start mobilising the transferred finger or toe. We apply a removable thermoplastic splint which will allow easier mobilisation of the fingers. Regular supervised physiotherapy is continued for 6 to 8 weeks. After that, we allow full movement of the transferred digit. However, we do warn the patient that recovery of sensations take a longer time and hence they should not hurt themselves by touching a very hot or a very cold object
Is physiotherapy essential? Will I need to do physiotherapy at Ganga Hospital or can I get it done elsewhere ?
Regular supervised physiotherapy is very important as it avoids stiffness of the transferred toe and it enables the thumb meeting the other fingers. Not many physiotherapists have experience in treating patients with toe transfer and hence we advice patients to have their physiotherapy done at Ganga Hospital at least in the initial stages. We have physiotherapists who are experienced in treating these patients.
How successful is this surgery ?
This surgery involves connection of blood vessels as small as 1 mm by microsurgery. We have a success rate of 96%. To prevent any complication intense monitoring is done for the first 5 days from the operation.
I come from a place that is far away from Coimbatore? How long will I need to stay in Coimbatore and do I need to stay in the hospital for the entire period ?
The patient needs to stay in the hospital for around 10 to 14 days after the surgery. We advise them to stay nearby so that they can come again 2 to 4 weeks from the day of discharge for K-wire removal. We advice patients to stay for at least 4 weeks after that so they can get regular physiotherapy. To summarise, the patient would need hospital stay for 2 weeks and stay near the hospital for another 6 weeks. We will try looking out for a place for the patients to stay outside the hospital if the patient desires..
What does the deformity “Cleft hand” mean?
Cleft hand is a rare congenital disability in which the child has an abnormal slit (Cleft) in the centre of hand with absent middle finger or more fingers.
Why does the Cleft hand happen?
Cleft hand is thought to happen due to mutations (errors) in genes which control hand formation in the embryo.
How common is this condition?
Cleft hands are rare, with an incidence of about 1 in 10,000 to 90,000 live births.
If we plan to have another child, what are the chances that the other child will also have it?
If a parent has it, there is a 50% chance of a child developing this condition.
What other problems can the child present?
In addition to clefts in hand and on foot, they can present with cleft lip and palate, protrusion of brain membrane ad rarely deafness.
Do all patients need surgery?
In some patients, the child may be able to do all activities with the hand and correction would be necessary to improve the appearance of the hand.
What are our goals of surgical treatment of cleft hand?
The goals of treatment of cleft hand surgery are to
Close the cleft and make sure that the child can use the hand effectively
Reorganise the skin and soft tissue
Stabilise or transfer the bones of the hand
Correct any other deformities of the fingers and thumb.
How can we treat cleft hand surgically?
The cleft hand can be treated surgically by closing the cleft and using the skin to augment the first webspace. Depending on each patient, the bony abnormalities can also be treated at the same time to facilitate the good movement of the fingers and thumb.
How long do we need to stay in the hospital for the procedure?
The child would need 3 to 4 days of stay in the procedure.
How is the patient managed post-operatively?
An above elbow cast is applied. Dressing under anaesthesia is done at 2 weeks. The wounds are expected to heal by then. The sutures are removed, and a slab is applied. The slab is removed at 4 weeks from surgery, and the child is allowed to play.
Will the fingers grow after surgery? Will the child be able to use the hand normally after the procedure?
The fingers will grow after surgery, and the child can use the hand normally after surgery.
My child’s toes are also involved. Could you operate on my child for that as well? If so, will they be done the same day?
Surgery for a cleft in the foot is not done in the same sitting as that of the hand. Generally, children with cleft foot do not have problems in walking. Surgery for the cleft foot is done only in severe cases and is done as a separate procedure.
In addition to having a cleft hand, my child also has some fused digits. Can they be operated the same time for that as well?
Surgery for cleft hand and fusion of fingers is done separately with a gap of a minimum of 6 months.
Facts at a glance (The facts could vary as per each case and needs to be confirmed with the doctor)
| Surgery time | Type Of Anaesthesia | Hospital Stay | Children Resuming playing | Suture removal |
|---|---|---|---|---|
| 3 hours approximately | General anaesthesia | 2 to 3 days | After a month | On 12th postoperative day or at 2nd week |
What is macrodactyly?
Macrodactyly is a condition in which the patient's fingers or toes are abnormally large because of overgrowth of the bone or soft tissue

Why does this happen?
The reason why macrodactyly occurs is still unknown. This condition isn't inherited and isn't caused by anything that the mother ate or did during her pregnancy. Macrodactyly is associated with some vascular malformations and neurofibromatosis.
How common is macrodactyly?
The prevalence of macrodactyly is 2 per 100,000 live births.
If we plan to have another child, what are the chances that the other child will also have it?
There has been no genetic cause found to date. Hence the chance of the next child being affected is uncommon.
How does macrodactyly present?
Macrodactyly presents with an enlarged digit. The index and middle fingers are the most commonly affected fingers. The distal parts are affected more than the proximal parts. Macrodactyly is classified as either static or progressive. The static form usually presents at birth and grows in proportion to the other fingers. The progressive form is seen in early childhood and grows rapidly and disproportionately to the other digits. The enlarged digits can be very stiff and deviated. Although the fingers are huge, they are functionally disabling and may hinder the function of the other fingers.
How is this condition treated?
Each finger is different and needs to be treated differently. An X-ray is taken, the patient is clinically examined, and the goals of the treatment and the treatment plan is discussed in detail with the parents of the child. Macrodactyly can be treated by different means like
Soft tissue Debulking
The soft tissue of the finger is debulked in stages to make the finger smaller.
Epiphysiodesis
The growth plate of the bones of the fingers is altered so that the growth in the fingers can be stopped.
Osteotomies
To correct the deviation of the fingers, the bones of the fingers can be cut at appropriate levels.
Shortening Procedures
The finger can be shortened so that the size of the finger is appropriate to the other fingers.
Ray amputation
When the finger is very big and functionally disabling, the whole finger is removed.
By reducing the size of the finger, will it function normally?
Surgery will help in making the finger look better and will also improve the functionality of the finger. However, it is challenging to make the finger resemble the normal finger.
If we decide to go in for amputation of the finger, will my child be able to function normally?
The hand functions well when the thumb meets another finger. Removal of a finger does not produce any functional disability, and the child will be able to do all activities that they were doing before. In fact, with the removal of the grossly enlarged finger, which may limit the motion of the other fingers, the child will be able to do all activities better than before.
At what age can the surgery be done?
The timing of surgery depends on how big the digit is. If the finger is very big, then we would like to see the child early. We may then do the surgery as early as 6 months. If not, we would like to do the surgery around 1 year of age. There is no upper limit in the age for correction of macrodactyly.
Do we necessarily need to undergo surgery?
Surgery for macrodactyly is a personal choice for the parents. Fingers which are only mildly enlarged need not undergo surgery. However, it is preferable to operate on fingers which are grossly enlarged to improve the appearance and the functionality.
What are the risks associated with the procedure?
Although the fingers with macrodactyly are large, the amount of blood supply to the fingers is only as much as any other typical finger and is not proportional to the size of the large finger. Hence there can be wound healing problems, partial blackening of the skin and rarely blackening of the whole finger needing amputation of the finger after the operation. Generally, the fingers are stiff even before the operation and stiffness is also present later.
How is the child managed in the hospital and how long to stay in the hospital?
The patient may need to stay in the hospital for 2 to 3 days. We will do dressing under anaesthesia between 12th to 14th day. By 2nd week, the wounds are expected to heal well. We will remove the sutures, clean the wounds and apply a slab four By 4 weeks we remove all dressings and we will allow the child to play.
Will the fingers grow after surgery? Will the child be able to use the hand normally after that?
If epiphysiodesis is done, no further growth will be expected. When other procedures are done, the finger will grow until the other fingers stop growing.
The toes of my child are big. Are the options the same as that of the fingers?
The options of treatment for toes are the same as that of fingers. For toes, we prefer to amputate the toes as this gives a good result.
Facts at a glance (The facts could vary as per each case and needs to be confirmed with the doctor)
| Surgery time | Type Of Anaesthesia | Hospital Stay | Children Resuming playing | Suture removal |
|---|---|---|---|---|
| 2 hours approximately | General anaesthesia | approximately 2 to 3 days | After 4 weeks incase of debulking and after 6 weeks in case of epiphysiodesis | On 12th to 14th day |
Where is the Thoracic Outlet?
The thoracic outlet is a closed space within the lower part of the neck through which the nerves and blood vessels of the upper limb pass.
What is Thoracic Outlet Syndrome (TOS)?
Thoracic Outlet Syndrome is a condition in which the nerves (Neurogenic TOS) or the blood vessels (Vascular TOS) supplying the upper limb are compressed by structures at the level of the thoracic outlet.
Why does Thoracic Outlet Syndrome occur?
Thoracic Outlet Syndrome occurs due to several factors such as an abnormally long rib (Cervical Rib), hypertrophy of muscles around the lower neck, drooping shoulders, wrong posture, pregnancy or trauma.
How do patients with Thoracic Outlet Syndrome present?
Patients with TOS present with altered (Pins and needles) or absent sensation over the fingers, weakness, fatigue, heaviness in the hand and arm, fatigue in the upper limb on working, bluish discolouration of the fingers and even blackening of the fingers in some cases.
How are patients with thoracic outlet obstruction diagnosed?
Patients with TOS are diagnosed based on a detailed history, clinical examination by some tests and if needed, radiological investigations like X-ray, CT scan and nerve conduction studies.
What happens if the patient is left untreated with this condition?
During the course of the disease, initially, the symptoms may occur with the arms in an overhead position and go away with the arms by the side. As time goes on, symptoms often occur more frequently and in all positions. The numbness of the fingers can progress into absent sensations, grip in hand can be significantly reduced hampering day-to-day activities, and there can be blackening of the fingers.
How is this condition treated?
This condition can be treated by both medical and non-medical means. Initially exercises to strengthen and stretch the shoulder muscles can be done to increase the size of the thoracic outlet and decrease the pressure of the blood vessels and nerves in the thoracic outlet. If the symptoms do not subside by non-operative means, then surgery is indicated. An incision is made just above the collar bone and the structures compressing and tethering the nerves, and the blood vessels to the upper limb such as a cervical rib, enlarged muscle or a band across the neck are released. In some cases, there can be damage to the subclavian artery. In those cases, the damaged part of the subclavian artery needs to be resected and interposed with an artificial graft. To access the vessel, we may have to divide the collarbone and plate it at the end.
I come from a place that is far away from Coimbatore. How long will I need to stay in Coimbatore, and do I need to stay in the hospital for the entire period?
Patients may need 2 to 3 days of hospital stay. Physiotherapy is initiated in this period. Sutures are removed 2 weeks from the initial surgery.
Facts at a glance (The facts shown are those of the majority and may change according to each patient)
| Duration of Surgery | Type Of Anaesthesia | Hospital Stay | Return to work | Suture removal |
|---|---|---|---|---|
| 3 hours | General anaesthesia | 2 to 3 days | 2 - 4 weeks | 2 weeks |
What is De Quervain’s disease?
De Quervain’s Disease is a painful condition at the base of the thumb which occurs due to the inflammation of the tendons that control the movement of the thumb. The pain is increased by gripping and rotating the wrist.

Why does De Quervain’s disease occur?
There are two tendons, namely the Extensor Pollicis Brevis (EPB) and Abductor Pollicis Longus (APL) which tend to move the thumb away from the palm. These two tendons pass through a small tunnel. When the tendons get swollen due to repetitive strain or when the tunnel is too small for the tendons, the tendons get inflamed, which produces pain.
In which group of people is De Quervain’s disease more common?
Workers who perform rapid repetitive activities like grasping, pinching, pushing and pulling are at high risk. De Quervain’s disease is commonly seen in pregnant women, probably due to fluid retention secondary to hormonal changes. This problem is also common in professionals who use the computer mouse, trackball and type a lot.
How does De Quervain’s present?
De Quervain’s disease commonly presents with a sudden sharp pain over the base of the thumb, especially while doing certain activities that involve the thumb moving towards the palm.
How will you diagnose De Quervain’s disease?
De Quervain’s disease is diagnosed clinically with some tests that are performed by the doctor in the clinic. Usually, no further investigations are needed to clinch the diagnosis.
How is De Quervain’s disease treated?
We often treat patients non surgically first as many patients get well by this method itself.
Non-surgical methods :
Initially, the thumb is supported by a splint which prevents the thumb from unduly moving. We advise the patients to keep their hand elevated above the level of heart and encourage the movement of the other fingers of the hand. Rest and elevation help to reduce oedema and inflammation in that area. Steroid injections can help some people to reduce the inflammation, although it is said that it can weaken the tendons.
Surgical method :
If the pain has not subsided even after 3 weeks of non-surgical methods, surgery is recommended. An injection is given in the armpit or the shoulder so that the procedure is painless. A 1 cm incision is made near the base of the thumb, and the tight tunnels of the compartments are released, and the skin is sutured. The dressing is applied along with a splint.
How is the patient managed post-operatively?
The patient is discharged the same day, or they are discharged the next day. The patient is advised to keep the hand elevated. The sutures can be removed in 12 to 14 days from the date of surgery. A mild compression garment is given to reduce any oedema. The patient can start using the hand from the next day.
If De Quervain’s disease is left untreated what can happen?
Left untreated, the movement of the thumb can be very painful, and this can limit pinching, gripping and many other activities of daily living.
Will this come back again after the surgery?
It is very unlikely to get the pain back at the same site as we have surgically released the tunnel.
Facts at a glance (The facts could vary as per each case and needs to be confirmed with the doctor)
| Surgery time | Type Of Anaesthesia | Hospital Stay | Resume cooking | Resume writing | Resume lifting heavy objects | Suture removal |
|---|---|---|---|---|---|---|
| Twenty minutes | Axillary or brachial plexus block | Few hours or 1 day | The very next day | The very next day | After 2 weeks | After 2 weeks |