Department Overview
The Department of Physiotherapy at Ganga Medical Hospital strives to provide quality patient-centred care that focuses on optimising functional ability and independence of patients according to the highest standards of care. The services involve timely, effective and efficient treatment techniques as well as education to patients by a team of well informed, dedicated and committed physiotherapists. The mission of our physiotherapy doctors in the department is to render comprehensive physiotherapy to services in the areas of preventive, curative, promotive and rehabilitative physiotherapy based on clinical assessment, medical information and sound professional judgement with the ultimate aim of improving the quality of life of patients.
The Physiotherapy Department is organised under Four core specialities, which encompass the scope of physiotherapy practice namely:
- Inpatient and Out-Patient Orthopaedic Surgery, Rheumatology, Spine problems, Trauma care, Pain Management and Hand Therapy for both operative and non-operative patients.
- Rehabilitation: spinal cord injury, Stroke care and Neurology and cerebral palsy Rehabilitation
- Inpatient and Outpatient Plastic, Hand, Burns and micro Surgery, tendon injuries, replantation, nerve injuries, soft tissue repair and reconstruction, brachial plexus injury and spastic hand.
- Cardio-respiratory care: Surgical Respiratory, Medical Respiratory, Invasive and Non- Invasive Ventilation in Intensive Care Unit(ICU).
All clinical areas are represented by senior physiotherapists who take responsibility for staff grade physiotherapists (who rotate through a variety of clinical areas), and students (the department is also a clinical placement centre for physiotherapy students from Various institutions). Currently, there are over 45 physiotherapists, 3 physiotherapy assistants providing physiotherapy services for patients in Ganga Hospital.
In-Patient Care:
Our team of best physiotherapist's provides specialized treatment for patients who have undergone a wide range of procedures in Orthopedics, Spine, Replacement and neurological surgery. Patients receive appropriate treatment and rehabilitation and, in preparation for their discharge, are given advice and a Programme of exercises. Local patients may then continue physiotherapy on an out-patients basis if needed.
Out-Patient Care:
Our department provides the necessary training to meet the total range of patient care responsibilities involved in preventing disabilities and promoting restoration of function to the physically impaired, including Musculoskeletal, Neuromuscular disorders that interfere with the physical function. Our management includes prescription of
Exercise Therapy with the aid of
- Continuous Passive movement device
- Electronic Cervical and Lumbar Traction Unit
- Moist Heat Therapy and Paraffin Wax Bath
- Manual Therapy
Electrotherapy treatment such as
- Inferential Therapy
- Transcutaneous Electrical Nerve stimulation Therapy
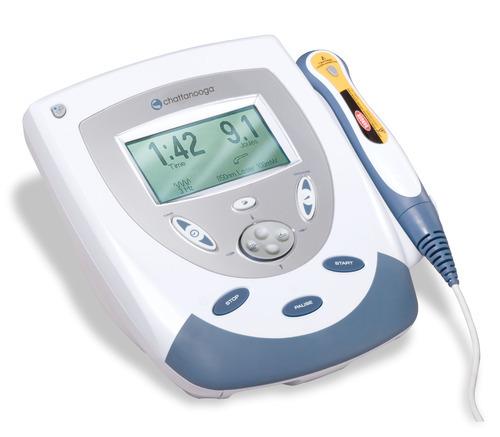
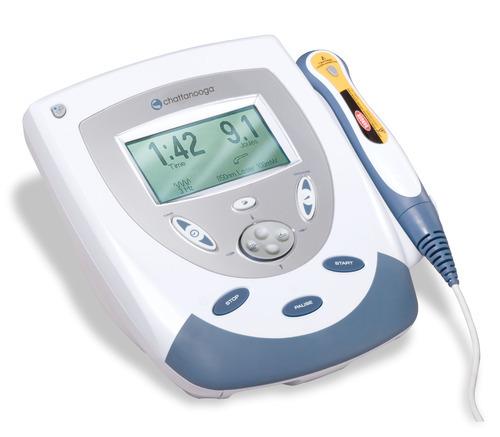
- Ultra-sound therapy
- Muscle Stimulation.

Orthopaedic Physiotherapy Patients
| 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 |
|---|---|---|---|---|---|---|
| 44,096 | 44,478 | 47,854 | 49,445 | 54,149 | 54,197 | 27,664 |











Technology

Wax therapy in physiotherapy is one of the methods used by physiotherapists to cure body pain by applying paraffin wax, which is considered as one of the most effective ways of applying heat and treating body pain. It is among the latest trends of 'feel good' spa that people are opting for.
Paraffin wax for physiotherapy helps in reducing body stiffness and pain and also moisturizes the skin and regulates blood circulation in the body. Paraffin wax has an exceptionally high warmth limit, which means it can ingest and hold an extraordinary measure of warmth.
A paraffin wax shower exploits paraffin's kindness holding limit in a straightforward procedure called heat transfer. As it liquefies, it turns out to retain heat. At that point, when a hand, foot, or other zone is dunked into the warm shower, the paraffin rapidly changes into a strong, moving the warmth to the plunged region. That's the very reason for the use of paraffin in physiotherapy wax treatment.
Transcutaneous electrical nerve stimulation (TENS) is a non-invasive peripheral stimulation technique used to relieve pain. During TENS pulsed electrical currents are delivered across the intact surface of the skin to activate underlying nerves. Patients can self-administer TENS and titrate dosage as required because there is no potential for overdose and there are few side effects or drug interactions.
Maximal analgesia occurs when TENS generates a strong but non-painful electrical paraesthesia beneath the electrodes. Effects are generally rapid in onset and offset so patients are encouraged to administer TENS as needed and throughout the day.
Interferential Therapy or (IFT) is a type of electrotherapy treatments that use electric currents to stimulate tissue which provides pain relief, reduction of swelling and many other health benefits. It is rather a generic means of stimulation – the machine can be set up to act more like a TENS type device or can be set up to behave more like a muscle stimulator – by adjusting the stimulating (beat) frequency. It is often regarded (by patients) to be more acceptable as it generates less discomfort than some other forms of electrical stimulation.
Selection of a wide frequency sweeps has been considered less efficient than a smaller selective range in that by treating with a frequency range of say 1-100Hz, the effective treatment frequencies can be covered, but only for a relatively small percentage of the total treatment time. Additionally, some parts of the range might be counterproductive for the primary aims of the treatment.
The are 4 main clinical applications for which IFT appears to be used:
Pain relief
Muscle stimulation
Increase local blood flow
Reduction of oedema

Faradic Current
Faradic is an interrupted direct current that has a frequency of 50:100Hz with a pulse duration from 0.1-1 ms. This frequency and duration cause contraction and relaxation in innervated (nerves intact) muscles. It does not work on muscles that are denervated muscle; to cause the same effect a short pulse duration would be required. When applying faradic stimulation, the stimulation of the sensory nerve can result in the patient experiencing a pricking sensation due to the short duration of the pulse. The stimulated nerve causes a reaction in the motor fibres which makes the muscle contract.
Galvanic Current
Galvanic current is interrupted direct current has frequency 30 Hz with pulse duration 1 ms and more. This type of current used for muscle not have the nerve because of injury of the nerve. When applying galvanic, the denervated muscle responds to this stimulus because of the long pulse duration. The denervated muscle does not respond to faradic because pulse duration is short.

Traction is a tool that is useful only for conditions where decompression is required. Examples are nerve impingements and disc prolapses. As poor posture, movement patterns and muscle strength are the primary causes for disc prolapses and impingements, traction alone may reduce the pain but is not a long term solution to the rehabilitation of disc prolapses and nerve impingements.
The pressure within the structures, such as the disc, reduces as the spinal structures are gently pulled away from each other. As such, the space from which nerves exit the spinal cord increases. Therefore, traction is suitable for conditions with compressive stress within the spinal structures like disc proplapses and nerve impingements.Correcting posture, movement patterns and building core strength are the long-term solutions to back pain.
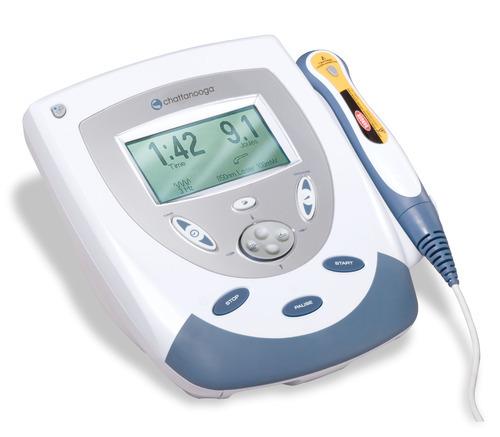
Sound waves are longitudinal waves consisting of areas of compression and rarefaction. Particles of a material, when exposed to a sound wave will oscillate about a fixed point rather than move with the wave itself. As the energy within the sound wave is passed to the material, it will cause oscillation of the particles of that material. Clearly any increase in the molecular vibration in the tissue can result in heat generation, and ultrasound can be used to produce thermal changes in the tissues, though current usage in therapy does not focus on this phenomenon.
In addition to thermal changes, the vibration of the tissues appears to have effects which are generally considered to be non thermal in nature, though, as with other modalities (e.g. Pulsed Shortwave) there must be a thermal component however small. As the US wave passes through a material (the tissues), the energy levels within the wave will diminish as energy is transferred to the material. The energy absorption and attenuation characteristics of US waves have been documented for different tissues.
The application of therapeutic ultrasound can influence the remodelling of the scar tissue in that it appears to be capable of enhancing the appropriate orientation of the newly formed collagen fibres and also to the collagen profile changes, thus increasing tensile strength and enhancing scar mobility
Therapeutic exercise is one of the core skills upon which the profession of physiotherapy is based on. By considering definitions of therapeutic exercise, physical activity and exercise, it is possible to see that, although therapeutic exercise contains the components of both physical activity and exercise, it also provides a systematic exercise programme for remediation of impairments and improvement of function.
Exercise is a physical activity that is planned and is performed with the goal of attaining or maintaining physical fitness. Physical fitness is a set of traits that allows an individual to perform physical activity
Therapeutic exercise include:
Aerobic and endurance conditioning and reconditioning
Agility training
Body mechanics training
Breathing exercises
Coordination exercises
Developmental activities training
Movement pattern training
Neuromotor development activities training
Neuromuscular education or reeducation
Perceptual training
Range of motion exercises and soft tissue stretching
Relaxation exercises
Strength, power, and endurance exercises
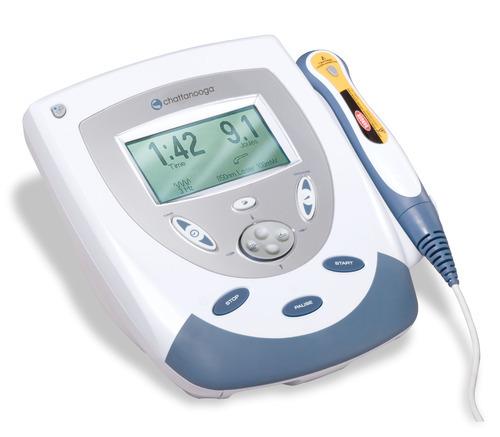
Sound waves are longitudinal waves consisting of areas of compression and rarefaction. Particles of a material, when exposed to a sound wave will oscillate about a fixed point rather than move with the wave itself. As the energy within the sound wave is passed to the material, it will cause oscillation of the particles of that material. Clearly any increase in the molecular vibration in the tissue can result in heat generation, and ultrasound can be used to produce thermal changes in the tissues, though current usage in therapy does not focus on this phenomenon.
In addition to thermal changes, the vibration of the tissues appears to have effects which are generally considered to be non thermal in nature, though, as with other modalities (e.g. Pulsed Shortwave) there must be a thermal component however small. As the US wave passes through a material (the tissues), the energy levels within the wave will diminish as energy is transferred to the material. The energy absorption and attenuation characteristics of US waves have been documented for different tissues.
The application of therapeutic ultrasound can influence the remodelling of the scar tissue in that it appears to be capable of enhancing the appropriate orientation of the newly formed collagen fibres and also to the collagen profile changes, thus increasing tensile strength and enhancing scar mobility

Continuous passive motion (CPM) devices are used during the first phase of rehabilitation following a soft tissue surgical procedure or trauma. The goals of rehabilitation is control post-operative pain, reduce inflammation, provide passive motion in a specific plane of movement and protect the healing repair of tissue.
CPM is used following various types of reconstructive joint surgery such as knee replacement and ACL reconstruction. Its mechanisms of action for aiding joint recovery are dependent upon what surgery is performed. One mechanism is the movement of synovial fluid to allow for better diffusion of nutrients into damaged cartilage, and diffusion of other materials out; such as blood and metabolic waste products. Another mechanism is the prevention of fibrous scar tissue formation in the joint, which tends to decrease the range of motion for a joint.

It is a device used for exercise, consisting of a continuous moving belt on which to walk or run. One of the most popular types of home exercise equipment is the treadmill, which provides a straightforward, efficient aerobic workout. As strength and endurance are developed, the treadmill can be used for jogging and/or for interval training.
Exercise without pain
Promote cardiovascular and muscle health
Work on your gait
Reduce impact on your joints
Confidence

Swiss balls are large, heavy-duty inflatable balls with a diameter of 45 to 75 cm (18 to 30 inches). Swiss balls are one of today's top fitness tools - and for good reason! Using a Swiss ball will improve the strength of the abs and the lower back. Since the Swiss ball is unstable you have to constantly adjust your balance, which in turn will improve your balance, proprioception and flexibility. As an extra challenge you can use the exercise ball as a bench using free-weights to target those hard to reach stabilizer muscles. Swiss Ball Pro is more recommended for heavy strength training and body building
Proper Alignment
Great Abs
Muscle Strength and Endurance
Core Stability
Stretching
Losing Weight
Swiss balls offer you a fun, safe and highly effective way to exercise. They will last for a very long time and are inexpensive compared to other exercise equipment.

The mat program involves the patient in activities incorporating both movement and stability. They range from single movements, such as unilateral scapula motions, to complex combinations requiring both stabilization and motion, such as crawling or knee walking. The activities are done in different positions, for function and to vary the effects of reflexes or gravity. The therapist also chooses positions that can help control abnormal or undesired movements.
Mat treatment unites all the parts of the PNF philosophy. In this situation it is easy to begin with activities that are strong and pain free and work toward improving those functions that need improvement. Because the mat activities involve many parts of the body, irradiation from the strong parts is easier to achieve. Last (but not least) the work can be fun.
When working with an infant, it may be necessary to progress treatment using activities that suit the developmental level of the individual. With the adult patient more mature or advanced activities can be used before the more basic activities. Functional goals direct the choice of mat activities. An activity, such as getting from supine to sitting, is broken down and the parts practiced. As there are many different ways in which a person can accomplish any activity, treatments should include a variety of movements. For example, to increase trunk and leg strength, the patient may begin treatment with resisted exercises in sitting and side-sitting. The treatment then progresses to positions involving more extremity weight-bearing. As the patient’s abilities increase, exercises that combine balance and motion in bridging, quadruped, and kneeling positions are used.
With all functional activities, the patient learns:
Mobility - moving into a position or starting a movement
Stability - stabilizing (balance) in that position and controlling gravity
Mobility on stability - possibility to control a movement in any position in a stable position
Skill - all movements are possible, all body parts can be moved and controlled in all directions
Swiss balls offer you a fun, safe and highly effective way to exercise. They will last for a very long time and are inexpensive compared to other exercise equipment.
The role of the respiratory physiotherapist is to assist in clearing the airways of the patients, and maintaining and improving the integrity of the respiratory system. Treatment interventions include:
Positioning
Education
Manual and ventilator hyperinflation
Weaning from mechanical ventilation
Non-invasive ventilation
Percussion, vibration, suctioning
Respiratory muscle strengthening
Breathing exercises and mobilisation
Specialization
The Orthopaedic physiotherapy doctors in Coimbatore, at Ganga Medical Centre aim to providing support and recovery for the treatment of musculoskeletal ailments. We provide our patients with individualized and comprehensive physical therapy and rehabilitation programs. Our commitment to excellence begins with a focus on personalized attention. We recognize that each person has their own unique needs and desired outcomes. At the outset of care, each patient’s medical and physical history is assessed along with other lifestyle factors and a personalized treatment program is developed based on the patient’s injury, age, sport, and other lifestyle needs. We set treatment goals in order to develop the most effective customized physical therapy and rehabilitation plans possible.
We provide treatment to Back Pain(LBA), Neck Pain, Shoulder Pain, Elbow Pain, Hand and Wrist Pain, Hip Pain, Knee Pain, Sciatica Pain, Osteoarthritis, Ligament Injury, Ankle and Foot injury, Muscular Disease, Rehabilitation of Musculoskeletal Disorders, Rheumatoid Arthritis, other Chronic Pain Conditions. Customized treatment plans are designed to increase strength, restore range of motion and alleviate pain. Physiotherapy and rehabilitation programs are developed using the most effective treatment methods available, including:
- Advanced Manual Therapy Techniques
- Joint Mobilization
- Therapeutic Exercise
- Postural Correction
- Balance and Proprioception Training
- Strengthening, Flexibility and Mobility Training
- Post-Operative Rehabilitation
- Heat Therapy with safe Wax Bath Technique
- Home Exercise Programs and Handouts
- Ergonomic Advice
We are the best physiotherapist in coimbatore offering a specialized Rehabilitation unit for the Spine Injury Individuals has been developed by Ganga medical centre and hospital. Ganga Spine Injury and Rehabilitation centre is the largest dedicated rehabilitation centre in the country with 33 beds, a built-in space of 15750sq ft. We have a highly specialized multidisciplinary team of Spine & Orthopedic Surgeons, Physiotherapist, Occupational Therapist, Social Worker, Nurse, Psychologist, Peer Counselor, Vocational Trainer & Orthotist.
Ganga Spine Injury Rehabilitation Centre (GSIRC) is one of the most prominent and dedicated spinal injury rehabilitation in the country. When you or some you love is affected by a spinal cord injury, we understand how debilitating life can become physically and emotionally. At GSIRC, we aim to optimize recovery and effectively improve independence and quality of life of a Spinal Cord Injured (SCI) person, regardless of the severity of the injury. Our highly qualified and experienced team provide comprehensive and individualized rehabilitation for patients. We have rehabilitated more than 500 spinal cord injured patients until December 2017. GSIRC works in conjunction with the Spine Unit of Ganga Hospital, Coimbatore to fulfil rehabilitation requirements in the aftermath of surgical treatments of spinal cord injuries. We understand that spinal injuries can scar your life, and want to walk this difficult journey with you and show how you can live independently and positively for now on.
https://www.gangaspinerehab.org/
Hand Therapy helps patients in their recovery after they have had Hand Surgery. Ganga Medical Centre has a dedicated team of top physiotherapist in Coimbatore who are trained in Hand therapy. We work with patients on a one-on-one basis, assessing a patient, creating a plan for therapy, making custom splints and braces as needed and teaching exercises and other therapeutic techniques. Treatment may also be aimed at improving grip strength or range of movement. Conditions seen by this team include a whole range of disorders that affect both the bones and the soft tissues. These include osteoarthritis, finger fractures, tendon injuries, peripheral nerve injuries. Many of the Hand Therapy Team’s patients are referred post-operatively by the Hand Consultants. Patients are assessed and an individual treatment programme is developed and tailored to their needs. Treatment may include such things as joint mobilisation techniques, Tendon gliding exercises, strengthening work, ultrasound, desensitisation techniques, and tailor-made splints.
We are the best physiotherapy centre in Coimbatore for, Surgical Respiratory, Medical Respiratory, Invasive and Non- Invasive Ventilation in Intensive Care Unit(ICU).
The physiotherapists at Ganga Medical Centre extend their services to sports injuries, by providing health and fitness solutions as well as on the prevention of injury and illness. They possess the knowledge and experience for the promotion of wellness and prevention of injury, across many areas of medicine such as exercise physiology, biomechanics, nutrition, psychology, physical rehabilitation, epidemiology, physical evaluation and injuries. It is the goal of a Sports Medicine Specialist to improve the health of the individual engaged in a demanding physical sport.
Home Physiotherapy is the continuity of health care needs of the patient or individual ensuring access to appropriate physiotherapy services thus enhancing speedy recovery.
Benefits of Home Physiotherapy
- Receiving Physiotherapy treatment in the comfort of their own home
- Reduces financial cost to the patient
- Travelling time to patients is eliminated
- Patient convenient / Flexible timings
- Quality treatment at an affordable cost
- Physiotherapy at home allows the rest of the family to be involved in the treatment and gain a better understanding of the condition




 Department Overview
Department Overview Technology
Technology Specialization
Specialization