TUG FLAP
TUG flap (Transverse Upper Gracilis Flap)
What is TUG flap?
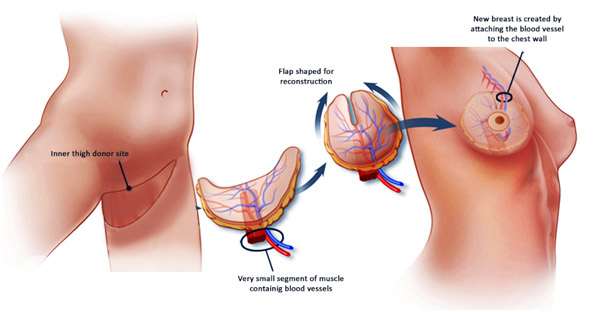
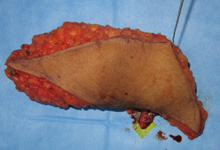
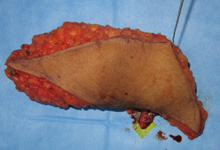
- The skin and fat along the upper inner thigh is taken along with gracilis muscle and it’s blood supply to constitute the Transverse Upper Gracilis (TUG) Flap. This flap is widely used for breast reconstruction.Gracilis is one of the many muscles in the inner thigh which is responsible for bringing the thigh towards the centre. As many muscles in the thigh can do the same action, taking this muscle leaves no functional problems. The skin and fat look like a “ melon slice” which can be made into a cone shape to form a soft and shapely breast. The peak of the cone becomes the nipple. The blood vessel accompanying the flap is then connected to the blood vessel in the chest by advanced microsurgery to form a nice breast of a good shape.
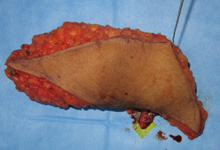
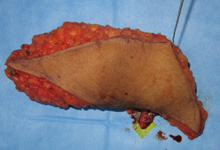
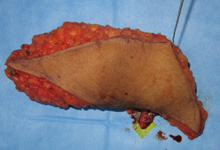
The TUG flap from the inner thigh is shaped like a breast by folding it
Primary nipple reconstruction is done

- For a patient who had breast cancer both sides, the breasts were removed both sides ,TUG flaps along with primary nipple reconstruction was done on both sides to make it look like breasts

- The final result after TUG flap reconstruction for both sides of the breast
When is TUG Flap preferred for breast reconstruction?
- DIEP flap is usually considered as the gold standard method of breast reconstruction wherein we take the excess skin and fat from the abdomen to make a breast. This is because of the versatility of the flap and favourable donor site.TUG flaps are usedfor breast reconstruction for the following reasons
- When the abdominal tissue can notbe used as in patients who have undergone abdominoplasty or other abdominal operations which can cause severe scarring
- It is also used in women who are very thin who do not enough excess skin and fat in the abdomen.
- It is also used in women who do not have good blood vessels supplying the abdomen
- TUG flaps can withstand radiotherapy well. Hence it can be used in people who need to undergo radiotherapy
What are the advantages of TUG flap?
- The TUG flap can give good reconstruction for breasts of small volume
- Since it is the patient’s owntissues, it can withstand radiotherapy well,and there are fewer complications associated with radiotherapy
- Since we use the patient’s tissues, it can result in the natural ptosis of the breast and give a superior cosmetic outcome
- Nipple reconstruction can be done at the same time as the TUG Flap
- The donor site is not visible as it is taken from the upper inner thigh. There is only a linear scar around the groin
- It can also be used to add volume to an already existing breast tissue as in partial breast reconstruction after breast conservative therapy
- It can also be used to add volume to the breast when combined with other flaps
Can breast reconstruction with this flap be done while removing breast cancer?
- Breast reconstruction with the TUG flap is ideally done during the same sitting as the removal of the breast cancer. When the reconstruction is done together with the removal of the breast cancer, most of the skin can be preserved if it has not been involved with breast cancer and can give a good result for breasts with a small volume. It can also be done in a delayed sitting. However, as the skin is not preserved, we may have to use TUG flaps from both sides to give a breast of a good shape.
What is done during the preoperativeassessment?
- Before the operation, we evaluate the status of investigations and treatment of breast cancer. If the patient had not been evaluatedearlier, we do the necessary investigations for breast cancer. We would then assess the volume, ptosis, size of the breast and the donor sites for autologous reconstruction like the thigh, abdomen and back. We may take a CT Angiogram to know the position of the vessels. We would then discuss with the patient and her relatives about what needs to be done for breast cancer, how we can reconstruct the breast the best way and answer any doubts that the patient and her relatives may have.
What will be the post operative care needed?
- The patient is evaluated in the microsurgical bay wherein the patient is near the operation theatre so that the doctors and specialised nurses can frequently visit the patient and look out for the viability of the flap and look out for haematoma. On the third day, we will mobilise the patient and try to make the patient sit down and slowly we will make the patient walk as soon as the patient is comfortable. We will also check the amount of fluid in the drains that are used to remove the excess fluid in the breast and the donor site in the thigh. When the amount of fluid in the drains reduce,we will remove the drains. Once all the drains are removed,and the patient can walk well, we will discharge the patient back home. The patient will need to stay in the hospital for a week. After discharge, we will see the patient once every week for two weeks. After the wounds heal,the patient is sent for chemotherapy if she needs it for her breast cancer treatment. Generally, the patient is sent for chemotherapy 3 to 6 weeks from the day of operation.
What could be the complications of TUG flap?
- Fortunately, the complications of TUG flap are not very common. Any surgical procedure can have its complications. As it our duty to inform our patients of the complications that can arise we are enumerating the complications of the TUG flap namely
- Wound healing problems As in any surgical procedure, there can be wound healing problems. Generally, they are addressed by few dressings.
- Flap loss The blood vessel of the flap is connected to the blood vessel in the chest by advanced microsurgery. In spite of all our efforts, there can be a block in the blood flow through the connection. That is the primary reason why we keep the patient near the operation theatre so that the doctors and specialised nurses can see the patient and correct it early. If we detect any problem in the blood flow in the connection, we immediately take the patient to the operation theatre and try to correct it. Mostly we can correct the problem. However, at times, we may not be able to correct itand we may end up losing the flap. In that instance, we wait for the wounds to settle and can again do another procedure for breast reconstruction after the wounds heal well. This complication is, fortunately less and is seen about 2 to 3%.
- Seroma Seroma is a collection of serous fluid under the flap or in the donor site. If the amount of serous collection is less, the patient can be observed once every week. If the amount of serous collection is more, the collection can be aspirated under ultrasound guidance.
- Haematoma A haematoma is a collection of blood. If the amount of haematoma is less, then the patient can be repeatedly observed as it will settle down by itself. However if the collection of blood is more then we may take the patient to the theatre to remove the collected blood as it may compromise the blood flow to the flap.