THYROID CANCER
What is a Cancer?
- Cells are the basic building blocks of the tissues and organs of our body. Usually, these cells divide to make new cells in a controlled manner, and beyond a point, the cells are replaced with new cells. This is how our bodies grow, heal and repair. Sometimes, this orderly growth of cells can go wrong due to the mutation or sudden change in the genes which control how cells behave. This can make the cells divide abnormally producing more and more abnormal cells, forming a lump called a tumour. These cells cannot stay together, can easily detach from each other and spread via direct contact, lymphatics and bloodstream to different organs in the body.
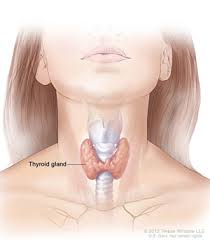
What is the thyroid gland?
- The thyroid is a small butterfly-shaped gland present in front of the neck. It produces a hormone called thyroxine which affects the growth, development and function of almost all the cells in the body.
How common is thyroid cancer?
- Thyroid cancer accounts forn1.6 % of all cancers in India( 1 to 2 per 1 lakh population). Thyroid cancer ranks 19th among all cancers in India.
What are the Risk Factors of Thyroid cancer?
- Most thyroid cancers occur sporadically without any particular reason that one can find. However, some patients may have a family history and a history of head and neck radiation
How is thyroid cancer identified?
- Thyroid cancers present mainly as swelling in front of the neck, which moves up and down with swallowing. The other common symptoms are swellings in the neck, inability to swallow, difficulty breathing, and hoarseness of voice. They may rarely present as bone pain, loss of weight and appetite.
What is an FNAC of the thyroid?
- Fine Needle Aspiration Cytology (FNAC) is a test that helps to know whether the patient has cancer or not. In this test, a needle is injected multiple times into the tumour or the lymph nodes under negative pressure, and few cells are aspirated into the syringe. If the tumour or the lymph node is not easily palpable, it can be done under ultrasound guidance. The microscope analyses these cells to look out whether the tumour is benign or malignant. This is an office procedure, and this can be done in the clinic. There can be minimal discomfort for a few hours after the procedure.
What are the possible cytology reports and their corresponding treatment?
- Benign
Colloid Nodule /cyst- Observation / Surgery only if Symptomatic- Follicular Neoplasm
Hemithyroidectomy or removal of half of the thyroid gland (provided the opposite lobe is normal). If the final Histopathology turns out to be Follicular thyroid cancer, then the patient will need completion thyroidectomy or removal of the entire thyroid gland.- Papillary thyroid cancer
Total thyroidectomy- Medullary carcinoma thyroid
Thyroidectomy with Central compartment Neck Dissection.
Other rare cytology reports are Atypia of unknown significance, Follicular lesion of unknown significance and anaplastic thyroid cancer. Treatment decisions will be made on a case to case basis.
What are the other tests that may be require
The other tests that may be required are
- Thyroid function tests
A simple blood test is done to know whether the thyroid hormone produced is within the normal limits. If the thyroid hormone production is either lower or higher, we might need to give some medications to correct thyroid hormone production.- Examination of vocal cords ( Laryngoscopy)
If there is a change in the voice, we might do a laryngoscopy to know whether the vocal cords that help voice production are functioning well.- CT / MRI neck
In some cases, to know the extension of the tumour and also to look for the presence of lymph nodes, CT/MRI neck may be done- Calcitonin and CEA
They are blood tests that may be done if it is a Medullary carcinoma of the thyroid.
What are the treatment options for thyroid cancer?
- Thyroid cancers are most commonly treated by surgery. Depending on each case, we might use other methods such as TSH suppression therapy and Radioiodine therapy. Rarely radiotherapy, chemotherapy and targeted therapy may be used in advanced disease.
What are the surgeries done for thyroid cancer?
- Hemithyroidectomy
- Total thyroidectomy
- Neck dissection ( Central compartment neck dissection & Posterolateral Neck dissection.)
What is Hemithyroidectomy, and when is it done?
- Hemithyroidectomy is the removal of one half of the thyroid gland(one lobe of the thyroid gland along with isthmus). It is done for benign diseases, Follicular adenoma and selected early cancers. The advantage of hemithyroidectomy is that patients can avoid lifelong thyroxin and calcium supplementation.
What is Total thyroidectomy, and when is it done?
- Total thyroidectomy is the removal of the entire thyroid gland. It is the most common procedure done for thyroid cancers.
What is neck dissection, and when do we do Neck dissection?
- Neck dissection is the removal of the lymph nodes which are at high risk of cancer spread. Neck dissection is done when the lymph nodes are detected by clinical examination and ultrasound. In medullary carcinoma thyroid, the central compartment neck dissection is done along prophylactically (Even if nodes are not detected clinically or by ultrasound).
How is the scar after the thyroidectomy operation?
- The scar after a thyroidectomy operation is horizontal and merges along with the skin folds in the neck. They usually heal very well. Rarely they may present with hypertrophic scars, which might need some massaging of the scar and silicon sheets.
Facts at a glance about surgery and post-operative instructions: ( May vary from person to person)
| Type of Anaesthesia | General Anaesthesia |
|---|---|
| Surgery Time | 2 - 3 hours |
| Hospital Stay | 2 - 5 days |
| Mobilisation | 1st day |
| Drain removal | 1st or 2nd day |
| Normal diet | 1st day |
| Suture removal | No suture removal required |
| Self-care | 5 days |
| Full recovery | 2 weeks |
| Return to work | 3 weeks |
What are the complications of surgery?
- Transient Hypocalcaemia ( 20%)
The calcium levels may become low in some individuals for a short time. The parathyroid glands responsible for the calcium levels in the blood are close to the thyroid glands. These parathyroid glands might not work appropriately after surgery for a while. We tend to prevent this by using advanced technologies like Indocyanine green dye to identify parathyroid glands. The patients may need supplementation with calcium tablets till the calcium levels stabilise.- Voice change ( 1%)
This is a rare possibility that the voice can change after surgery. This can happen due to injury to the recurrent laryngeal nerve that is close to the thyroid gland. This complication is not common in our hands as we have experienced surgeons performing the operation, and we also use nerve monitoring to identify the nerves during surgery.- Bleeding & Infection
These are rare complications that can happen after any surgery- Hypertrophic scar
The scar after a thyroidectomy operation is horizontal and merges with the neck's skin folds. They usually heal very well. Rarely they may present with hypertrophic scars, which might need some massaging of the scar and silicon sheets.
What is Radioactive Iodine therapy?
- Radioactive Iodine therapy is given to patients after thyroidectomy surgery to prevent a recurrence. The thyroid gland and thyroid cancers preferentially tend to take up iodine compared to the other parts of the body. Radioactive material tagged with iodine is called Radioactive Iodine therapy. This helps to identify and destroy any residual thyroid gland or thyroid cancer. All patients with Intermediate and high risk will need Radioactive Iodine therapy. Risk stratification is based on age at diagnosis, biopsy report after total thyroidectomy, uptake in low dose scan and thyroglobulin values.
Is there any preparation involved before Radioactive Iodine treatment?
- Avoid taking thyroxine medication 6 weeks before radioactive iodine treatment
- Avoid iodine-rich food such as seafood and dairy products 1 week before treatment No other special preparation is required.
How is Radioactive Iodine treatment performed?
- Radioactive iodine is usually taken by mouth. As the dose given is low in low-risk patients, the patient will be discharged the same day after taking the scan. As the dose given is higher in intermediate or high-risk patients, the patient may be admitted in isolation, monitored and discharged after a few days once the dose falls to the permissible level.
What are the adverse effects of Radioactive Iodine therapy?
The adverse effects of radioactive iodine therapy usually subside in a few days
- Pain and swelling of salivary glands.
- Dry mouth.
- Low sperm counts.
- Very rarely second malignancy
Are there any special instructions to avoid after Radioactive Iodine therapy?
The adverse effects of radioactive iodine therapy usually subside in a few days
- Ladies are advised not to get pregnant 6 to 12 months after radioactive iodine treatment as the ovarian follicles may not be mature.
- Lactating mothers are advised to postpone the radioactive iodine treatment and done after lactation.
- Men are advised not to beget children for 3 months as the sperms may not be mature.
What is the chance of cure in Thyroid cancers?
The possibility of survival depends on the cancer stage, site of involvement, grade of the tumour and the patient's compliance with the treatment. The survival of patients with cancer is generally denoted as 5-year survival, wherein the percentage of people surviving at the end of 5years after a cancer diagnosis is noted down. This is given in the tabular column below.
5-year survival rate for Thyroid cancers.
Papillary Follicular Medullary Anaplastic Limited to thyroid 100% 100% 100% 31% Beyond thyroid or Nodal disease 99% 96% 90% 12% Distant spread 78% 63% 39% 4%
What is TSH suppression therapy?
- TSH ( Thyroid stimulating Hormone) is a hormone produced in the body that helps grow thyroid cancers. This production of TSH can be suppressed by giving higher doses of thyroxine hormones. The TSH level is monitored in frequent intervals, and the dose is adjusted accordingly.
What are the blood test done during Follow up?
TSH ( Thyroid Stimulating Hormone)
- TSH is a hormone produced in the body that can facilitate the growth and spread of thyroid cancers. We would like to keep it at a low level. We would like to monitor this level every 3 months for the first 2 years and then periodically lifelong.
- Thyroglobulin & Anti thyroglobulin antibody These are tumour markers that help to identify thyroid cancer recurrence early.