SALIVARY GLANDS CANCER
What is a Cancer?
- Cells are the basic building blocks of the tissues and organs of our body. Usually, these cells divide to make new cells in a controlled manner, and beyond a point, the cells are replaced with new cells. This is how our bodies grow, heal and repair. Sometimes, this orderly growth of cells can go wrong due to the mutation or sudden change in the genes which control how cells behave. This can make the cells divide abnormally, producing more abnormal cells, forming a lump called a tumour. These cells cannot stay together, can easily detach from each other and spread via direct contact, lymphatics and bloodstream to different organs in the body.
What are salivary glands?
- There are 3 pairs of major salivary glands in our body, including the parotid gland located in the cheek, submandibular glands located below the jaw bone and sublingual glands located below the tongue. Apart from the 3 pairs of major salivary glands, numerous minor salivary glands are in the lip, mouth, and upper aerodigestive tract. The primary function of salivary glands is to produce saliva, which helps form the food bolus, digestion of food, keeps the mouth moist, and has an anti-microbial effect.
What are the signs and symptoms of a salivary gland tumour?
- Swelling in the face and neck
- Pain
- Facial nerve palsy in which the muscles of expression in the face does not function well
- Difficulty in swallowing
How common are Salivary gland Neoplasms?
- Salivary gland neoplasms are rare tumours that account for only 3-4 % of all head and neck neoplasms. Most commonly seen in the parotid gland.
How can we diagnose salivary gland neoplasms?
- A detailed clinical history and a thorough clinical examination are made for each patient. CT Scan or MRI scan may be done to assess the extent of the spread of the tumour. Ultrasound-guided biopsy/ FNAC might be taken to confirm the diagnosis of salivary gland neoplasms.
What are the risk factors of salivary gland Neoplasms?
- Most salivary gland neoplasms occur sporadically without any particular reason that one can find. Other probable causes are high usage of tobacco and alcohol and radiation exposure when young
What are the surgeries performed for salivary gland tumours?
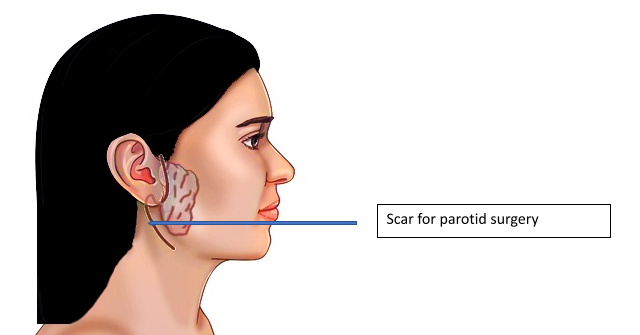
Parotid Gland
- Superficial Parotidectomy
Superficial parotidectomy is the most common parotid surgery done for the parotid gland. It is done commonly for benign parotid tumours and low grade parotid tumours. This involves removal of the parotid gland above the level of the facial nerve. Facial nerve is responsible for the movement of the muscles of expression of the face and there is usually no damage to the facial nerve by this surgery.
- Total or Radical Parotidectomy
Total or Radical Parotidectomy is done for malignant tumours of the parotid gland and high-grade tumours. Here the entire parotid gland is excised along with the facial nerve. As the facial nerve supplies the muscles of expression, the patient may not make any facial movements immediately on the corresponding side. So we might also reconstruct the nerves at the same time to get good movements of facial expression.
Sub Mandibular gland
- Radical Submandibular gland excision.
Radical Submandibular gland excision is the removal of the entire submandibular gland along with the surrounding structures and the draining lymph nodes
- Sublingual or other Minor salivary glands-
The tumours in the minor salivary glands are excised with a wide margin of 1 cm.
- Neck dissection
Malignant salivary gland tumours spread to the lymph nodes in the neck. So, along with the tumour, the lymph nodes in the neck are also removed. This is called lymph node dissection. The lymph nodes removed are sent for biopsy to know whether they are involved in malignancy. This lymph node dissection helps remove the affected lymph nodes and allows us to decide on the subsequent treatment whether chemotherapy or radiotherapy is needed.
What are the complications of salivary gland surgeries?
Although we make several efforts to reduce the complications, there can be some complications such as
- Facial nerve palsy
The facial nerve is a nerve responsible for the proper functioning of the muscles of expression of the face. While operating on malignant tumours of the parotid gland, the facial nerve might need to be sacrificed to clear the cancer cells properly. In these cases, the facial nerve is reconstructed with nerve grafts. In benign tumours of the parotid gland, the part of the parotid gland superficial to the facial nerve is removed. Facial nerve damage in these cases is overcome by good surgical expertise, nerve monitoring in selected instances, Ontable nerve grafts with microscopes and advanced plastic surgical techniques. Even though the facial nerve may not be damaged during surgery, the facial nerve may not work for a few days to weeks as the dissection is done close to the nerve. In these cases, the nerve recovers with time.
- Scar in the face.
The scar is hidden around the ear and then followed into the neck to be not very obvious. They usually heal very well. If they heal with hypertrophic scars, we use multiple techniques like scar massage, compression, LASER to heal them well.
- Bleeding & Infection
These are rare complications that can happen after any surgery. They settle with time.
- Sweating over parotid area while eating)- Frey’s Syndrome-
It occurs in approximately 10% of the patient. This happens as the nerves overlying the parotid are cut. Most cases settle on its own with medications and some injections. Rarely they need surgery.
When will radiotherapy be necessary?
Radiotherapy is used after surgery if the tumour is aggressive (High Grade), if lymph nodes in the neck are positive for malignancy, and sometimes in recurrent tumours.
Facts at a glance about surgery and post operative instructions: ( May vary from person to person)
| Type of Anaesthesia | General Anaesthesia |
|---|---|
| Surgery Time | 1 - 2 hours |
| Hospital Stay | 3 - 5 days |
| Mobilisation | 1st day |
| Drain removal | 1st or 2nd day |
| Normal diet | 1st day |
| Suture removal | No suture removal required |
| Self-care | 5 days |
| Full recovery | 2 weeks |
| Return to work | 3 weeks |